TYLENOL with Codeine
TYLENOL with CodeineCIII(acetaminophen and codeine phosphate) tablets, USP
FULL PRESCRIBING INFORMATION: CONTENTS*
- TYLENOL WITH CODEINE DESCRIPTION
- CLINICAL PHARMACOLOGY
- TYLENOL WITH CODEINE INDICATIONS AND USAGE
- TYLENOL WITH CODEINE CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- TYLENOL WITH CODEINE ADVERSE REACTIONS
- DRUG ABUSE AND DEPENDENCE
- OVERDOSAGE
- Signs and Symptoms
- Toxic Doses (for Adults)
- TYLENOL WITH CODEINE DOSAGE AND ADMINISTRATION
- HOW SUPPLIED
- Principal Display Panel-300 mg
- Principal Display Panel-400 mg
FULL PRESCRIBING INFORMATION
TYLENOL WITH CODEINE DESCRIPTION
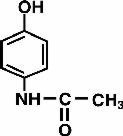
TYLENOL® with Codeine is supplied in tablet form for oral administration. Acetaminophen, 4’-hydroxyacetanilide, a slightly bitter, white, odorless, crystalline powder, is a non-opiate, non-salicylate analgesic and antipyretic. It has the following structural formula:
Each tablet contains:
Acetaminophen . . . . . . . . . . . . . . . .300 mg
No. 3 Codeine Phosphate . . . . . . . . .30 mg
(Warning: May be habit forming)
Acetaminophen . . . . . . . . . . . . . . . .300 mg
No. 4 Codeine Phosphate . . . . . . . . .60 mg
(Warning: May be habit forming)
In addition, each tablet contains the following inactive ingredients:
TYLENOL® with Codeine No. 3 contains powdered cellulose, magnesium stearate, sodium metabisulfite†, pregelatinized starch (corn), and modified starch (corn).
TYLENOL® with Codeine No. 4 contains powdered cellulose, magnesium stearate, sodium metabisulfite†, pregelatinized starch (corn), and corn starch. †See WARNINGS
CLINICAL PHARMACOLOGY
This product combines the analgesic effects of a centrally acting analgesic, codeine, with a peripherally acting analgesic, acetaminophen.
Pharmacokinetics
The behavior of the individual components is described below.
Codeine
Codeine is rapidly absorbed from the gastrointestinal tract. It is rapidly distributed from the intravascular spaces to the various body tissues, with preferential uptake by parenchymatous organs such as the liver, spleen, and kidney. Codeine crosses the blood-brain barrier and is found in fetal tissue and breast milk. The plasma concentration does not correlate with brain concentration or relief of pain; however, codeine is not bound to plasma proteins and does not accumulate in body tissues.
The plasma half-life is about 2.9 hours. The elimination of codeine is primarily via the kidneys, and about 90% of an oral dose is excreted by the kidneys within 24 hours of dosing. The urinary secretion products consist of free and glucuronide conjugated codeine (about 70%), free and conjugated norcodeine (about 10%), free and conjugated morphine (about 10%) normorphine (4%), and hydrocodone (1%). The remainder of the dose is excreted in the feces. At therapeutic doses, the analgesic effect reaches a peak within 2 hours and persists between 4 and 6 hours.
See OVERDOSAGE for toxicity information.
Acetaminophen
Acetaminophen is rapidly absorbed from the gastrointestinal tract and is distributed throughout most body tissues. The plasma half-life is 1.25 to 3 hours, but may be increased by liver damage and following overdosage. Elimination of acetaminophen is principally by liver metabolism (conjugation) and subsequent renal excretion of metabolites. Approximately 85% of an oral dose appears in the urine within 24 hours of administration, most as the glucuronide conjugate, with small amounts of other conjugates and unchanged drug.
See OVERDOSAGE for toxicity information.
TYLENOL WITH CODEINE INDICATIONS AND USAGE
TYLENOL® with Codeine (acetaminophen and codeine phosphate) tablets are indicated for the relief of mild to moderately severe pain.
TYLENOL WITH CODEINE CONTRAINDICATIONS
This product should not be administered to patients who have previously exhibited hypersensitivity to codeine or acetaminophen.
WARNINGS
In the presence of head injury or other intracranial lesions, the respiratory depressant effects of codeine and other narcotics may be markedly enhanced, as well as their capacity for elevating cerebrospinal fluid pressure. Narcotics also produce other CNS depressant effects, such as drowsiness, that may further obscure the clinical course of the patients with head injuries.
Codeine or other narcotics may obscure signs on which to judge the diagnosis or clinical course of patients with acute abdominal conditions.
Codeine is habit forming and potentially abusable. Consequently, the extended use of this product is not recommended.
TYLENOL® with Codeine (acetaminophen and codeine phosphate) tablets contain sodium metabisulfite, a sulfite that may cause allergic-type reactions including anaphylactic symptoms and life-threatening or less severe asthmatic episodes in certain susceptible people. The overall prevalence of sulfite sensitivity in the general population is unknown and probably low. Sulfite sensitivity is seen more frequently in asthmatic than in nonasthmatic people.
PRECAUTIONS
General
TYLENOL® with Codeine (acetaminophen and codeine phosphate) tablets should be prescribed with caution in certain special-risk patients, such as the elderly or debilitated, and those with severe impairment of renal or hepatic function, head injuries, elevated intracranial pressure, acute abdominal conditions, hypothyroidism, urethral stricture, Addison’s disease, or prostatic hypertrophy.
Ultra-Rapid Metabolizers of Codeine
Some individuals may be ultra-rapid metabolizers due to a specific CYP2D6*2x2 genotype. These individuals convert codeine into its active metabolite, morphine, more rapidly and completely than other people. This rapid conversion results in higher than expected serum morphine levels. Even at labeled dosage regimens, individuals who are ultra-rapid metabolizers may experience overdose symptoms such as extreme sleepiness, confusion, or shallow breathing.
The prevalence of this CYP2D6 phenotype varies widely and has been estimated at 0.5 to 1% in Chinese and Japanese, 0.5 to 1 % in Hispanics, 1 to 10% in Caucasians, 3% in African Americans, and 16 to 28% in North Africans, Ethiopians, and Arabs. Data are not available for other ethnic groups.
When physicians prescribe codeine-containing drugs, they should choose the lowest effective dose for the shortest period of time and inform their patients about these risks and the signs of morphine overdose (see PRECAUTIONS - Nursing Mothers).
Information for Patients
Codeine may impair the mental and/or physical abilities required for the performance of potentially hazardous tasks such as driving a car or operating machinery. Such tasks should be avoided while taking this product.
Alcohol and other CNS depressants may produce an additive CNS depression, when taken with this combination product, and should be avoided.
Codeine may be habit forming. Patients should take the drug only for as long as it is prescribed, in the amounts prescribed, and no more frequently than prescribed. Caution patients that some people have a variation in a liver enzyme and change codeine into morphine more rapidly and completely than other people. These people are ultra-rapid metabolizers and are more likely to have higher-than-normal levels of morphine in their blood after taking codeine, which can result in overdose symptoms such as extreme sleepiness, confusion, or shallow breathing. In most cases, it is unknown if someone is an ultra-rapid codeine metabolizer.
Nursing mothers taking codeine can also have higher morphine levels in their breast milk if they are ultra-rapid metabolizers. These higher levels of morphine in breast milk may lead to life-threatening or fatal side effects in nursing babies. Instruct nursing mothers to watch for signs of morphine toxicity in their infants including increased sleepiness (more than usual), difficulty breastfeeding, breathing difficulties, or limpness. Instruct nursing mothers to talk to the baby’s doctor immediately if they notice these signs and, if they cannot reach the doctor right away, to take the baby to an emergency room or call 911 (or local emergency services).
Laboratory Tests
In patients with severe hepatic or renal disease, effects of therapy should be monitored with serial liver and/or renal function tests.
Drug Interactions
This drug may enhance the effects of other narcotic analgesics, alcohol, general anesthetics, tranquilizers such as chlordiazepoxide, sedative-hypnotics, or other CNS depressants, causing increased CNS depression.
Drug and Laboratory Test Interactions
Codeine may increase serum amylase levels.
Acetaminophen may produce false-positive test results for urinary 5-hydroxyindoleacetic acid.
Carcinogenesis, Mutagenesis, Impairment of Fertility
No adequate studies have been conducted in animals to determine whether acetaminophen and codeine have a potential for carcinogenesis or mutagenesis. No adequate studies have been conducted in animals to determine whether acetaminophen has a potential for impairment of fertility.
Acetaminophen and codeine have been found to have no mutagenic potential using the Ames Salmonella-Microsomal Activation test, the Basc test on Drosophila germ cells, and the Micronucleus test on mouse bone marrow.
Pregnancy
Teratogenic Effects: Pregnancy Category C
Codeine
A study in rats and rabbits reported no teratogenic effect of codeine administered during the period of organogenesis in doses ranging from 5 to 120 mg/kg. In the rat, doses at the 120 mg/kg level, in the toxic range for the adult animal, were associated with an increase in embryo resorption at the time of implantation. In another study a single 100 mg/kg dose of codeine administered to pregnant mice reportedly resulted in delayed ossification in the offspring.
There are no adequate and well-controlled studies in pregnant women.
TYLENOL® with Codeine (acetaminophen and codeine phosphate) tablets should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Nonteratogenic Effects
Dependence has been reported in newborns whose mothers took opiates regularly during pregnancy. Withdrawal signs include irritability, excessive crying, tremors, hyperreflexia, fever, vomiting, and diarrhea. These signs usually appear during the first few days of life.
Labor and Delivery
Narcotic analgesics cross the placental barrier. The closer to delivery and the larger the dose used, the greater the possibility of respiratory depression in the newborn. Narcotic analgesics should be avoided during labor if delivery of a premature infant is anticipated. If the mother has received narcotic analgesics during labor, newborn infants should be observed closely for signs of respiratory depression. Resuscitation may be required (see OVERDOSAGE). The effect of codeine, if any, on the later growth, development, and functional maturation of the child is unknown.
Nursing Mothers
Acetaminophen is excreted in breast milk in small amounts, but the significance of its effect on nursing infants is not known. Because of the potential for serious adverse reactions in nursing infants from acetaminophen, a decision should be made whether to discontinue the drug, taking into account the importance of the drug to the mother.
Codeine is secreted into human milk. In women with normal codeine metabolism (normal CYP2D6 activity), the amount of codeine secreted into human milk is low and dose-dependent. Despite the common use of codeine products to manage postpartum pain, reports of adverse events in infants are rare. However, some women are ultra-rapid metabolizers of codeine. These women achieve higher-than-expected serum levels of codeine’s active metabolite, morphine, leading to higher-than-expected levels of morphine in breast milk and potentially dangerously high serum morphine levels in their breastfed infants. Therefore, maternal use of codeine can potentially lead to serious adverse reactions, including death, in nursing infants.
The prevalence of this CYP2D6 phenotype varies widely and has been estimated at 0.5 to 1% in Chinese and Japanese, 0.5 to 1% in Hispanics, 1 to 10% in Caucasians, 3% in African Americans, and 16 to 28% in North Africans, Ethiopians, and Arabs. Data are not available for other ethnic groups.
The risk of infant exposure to codeine and morphine through breast milk should be weighed against the benefits of breastfeeding for both the mother and baby. Caution should be exercised when codeine is administered to a nursing woman. If a codeine containing product is selected, the lowest dose should be prescribed for the shortest period of time to achieve the desired clinical effect. Mothers using codeine should be informed about when to seek immediate medical care and how to identify the signs and symptoms of neonatal toxicity, such as drowsiness or sedation, difficulty breastfeeding, breathing difficulties, and decreased tone, in their baby. Nursing mothers who are ultra-rapid metabolizers may also experience overdose symptoms such as extreme sleepiness, confusion, or shallow breathing. Prescribers should closely monitor mother-infant pairs and notify treating pediatricians about the use of codeine during breastfeeding (see PRECAUTIONS - General, Ultra-Rapid Metabolizers of Codeine).
TYLENOL WITH CODEINE ADVERSE REACTIONS
The most frequently observed adverse reactions include drowsiness, lightheadedness, dizziness, sedation, shortness of breath, nausea, and vomiting. These effects seem to be more prominent in ambulatory than in non-ambulatory patients, and some of these adverse reactions may be alleviated if the patient lies down. Other adverse reactions include allergic reactions, euphoria, dysphoria, constipation, abdominal pain, pruritus, rash, thrombocytopenia, and agranulocytosis.
At higher doses, codeine has most of the disadvantages of morphine including respiratory depression.
DRUG ABUSE AND DEPENDENCE
Controlled Substance
TYLENOL® with Codeine (acetaminophen and codeine phosphate) tablets are classified as a Schedule III controlled substance.
Abuse and Dependence
Codeine can produce drug dependence of the morphine type and, therefore, has the potential for being abused. Psychological dependence, physical dependence, and tolerance may develop upon repeated administration and it should be prescribed and administered with the same degree of caution appropriate to the use of other oral narcotic medications.
OVERDOSAGE
Following an acute overdosage, toxicity may result from codeine or acetaminophen.
Signs and Symptoms
Codeine
Toxicity from codeine poisoning includes the opioid triad of: pinpoint pupils, depression of respiration, and loss of consciousness. Convulsions may occur.
Acetaminophen
In acetaminophen overdosage, dose-dependent, potentially fatal hepatic necrosis is the most serious adverse effect. Renal tubular necrosis, hypoglycemic coma and thrombocytopenia may also occur.
Early symptoms following a potentially hepatotoxic overdose may include: nausea, vomiting, diaphoresis and general malaise. Clinical and laboratory evidence of hepatic toxicity may not be apparent until 48 to 72 hours post-ingestion.
In adults, hepatic toxicity has rarely been reported with acute overdoses of less than 10 grams or fatalities with less than 15 grams.
Treatment
A single or multiple overdose with acetaminophen and codeine is a potentially lethal polydrug overdose and consultation with a regional poison control center is recommended.
Immediate treatment includes support of cardiorespiratory function and measures to reduce drug absorption. Vomiting should be induced mechanically, or with syrup of ipecac, if the patient is alert (adequate pharyngeal and laryngeal reflexes). Oral activated charcoal (1g/kg) should follow gastric emptying. The first dose should be accompanied by an appropriate cathartic. If repeated doses are used, the cathartic might be included with alternate doses as required. Hypotension is usually hypovolemic and should respond to fluids. Vasopressors and other supportive measures should be employed as indicated. A cuffed endo-tracheal tube should be inserted before gastric lavage of the unconscious patient and, when necessary, to provide assisted respiration.
Meticulous attention should be given to maintaining adequate pulmonary ventilation. In severe cases of intoxication, peritoneal dialysis, or preferably hemodialysis, may be considered. If hypoprothrombinemia occurs due to acetaminophen overdose, vitamin K should be administered intravenously.
Naloxone, a narcotic antagonist, can reverse respiratory depression and coma associated with opioid overdose. Naloxone hydrochloride 0.4 mg to 2 mg is given parenterally. Since the duration of action of codeine may exceed that of the naloxone, the patient should be kept under continuous surveillance and repeated doses of the antagonist should be administered as needed to maintain adequate respiration. A narcotic antagonist should not be administered in the absence of clinically significant respiratory or cardiovascular depression.
If the dose of acetaminophen may have exceeded 140 mg/kg, acetylcysteine should be administered as early as possible. Serum acetaminophen levels should be obtained, since levels four or more hours following ingestion help predict acetaminophen toxicity. Do not await acetaminophen assay results before initiating treatment. Hepatic enzymes should be obtained initially and repeated at 24-hour intervals.
Methemoglobinemia over 30% should be treated with methylene blue by slow intravenous administration.
Toxic Doses (for Adults)
Acetaminophen: toxic dose 10 g
Codeine: toxic dose 240 mg
TYLENOL WITH CODEINE DOSAGE AND ADMINISTRATION
Dosage should be adjusted according to severity of pain and response of the patient.
The usual adult dosage is:
| Single Doses (Range) | Maximum 24–Hour Dose | |
| Codeine Phosphate | 15 mg - 60 mg | 360 mg |
| Acetaminophen | 300 mg - 1000 mg | 4000 mg |
Doses may be repeated up to every 4 hours.
The prescriber must determine the number of tablets per dose, and the maximum number of tablets per 24 hours, based upon the above dosage guidance. This information should be conveyed in the prescription.
It should be kept in mind, however, that tolerance to codeine can develop with continued use and that the incidence of untoward effects is dose related. Adult doses of codeine higher than 60 mg fail to give commensurate relief of pain but merely prolong analgesia and are associated with an appreciably increased incidence of undesirable side effects. Equivalently high doses in children would have similar effects.
HOW SUPPLIED
TYLENOL® with Codeine (acetaminophen and codeine phosphate) tablets are white, round, flat-faced, beveled edged tablet imprinted “McNEIL” on one side and “TYLENOL CODEINE” and either “3” or “4” on the other side and are supplied as follows: No. 3 - NDC 0045-0513-60 bottles of 100, NDC 0045-0513-80 bottles of 1000, NO. 4 - NDC 0045-0515-60 bottles of 100, NDC 0045-0515-70 bottles of 500.
Store TYLENOL® with Codeine tablets at 20° to 25°C (68° to 77°F). (See USP Controlled Room Temperature.)
Dispense in tight, light-resistant container as defined in the official compendium.
Manufactured by:
JOLLC
Gurabo, Puerto Rico 00778
Distributed by:
ORTHOMcNEIL
OMP DIVISION
ORTHO-McNEIL PHARMACEUTICAL, INC.
Raritan, New Jersey 08869
Revised January 2008
© OMP 2000 7518407
Cardinal Health
Zanesville OH 43701
IR7501008
Principal Display Panel-300 mg
NDC 0045-0513-60 (ORTHO-MCNEIL)
TYLENOL ®
with codeine Tablets No. 3
(acetaminophen and codeine phosphate)
100 tablets
300 mg/ 30 mg
CIII
Each tablet contains: codeine phosphate 30 mg, acetaminophen 300 mg
Ortho-McNeil
Rx ONLY
WARNING: Keep out of reach of children

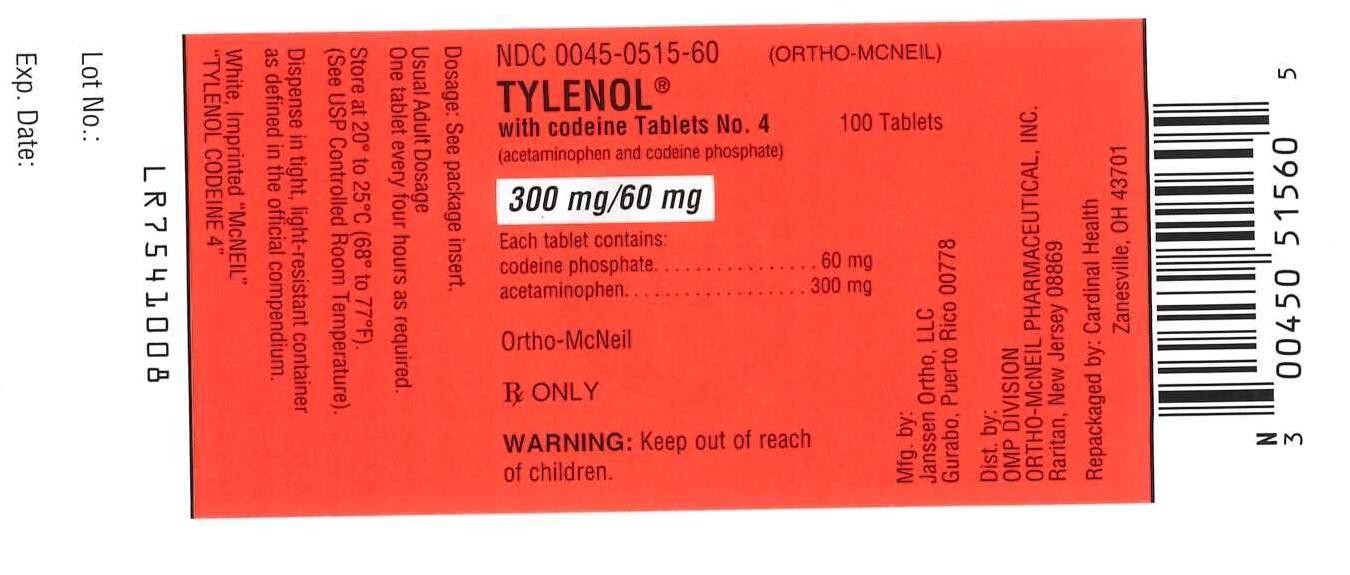
Principal Display Panel-400 mg
NDC 0045-0515-60 (ORTHO-MCNEIL)
TYLENOL ®
with codeine Tablets No. 4
(acetaminophen and codeine phosphate)
100 tablets
300 mg/ 60 mg
CIII
Each tablet contains: codeine phosphate 60 mg, acetaminophen 300 mg
Ortho-McNeil
Rx ONLY
WARNING: Keep out of reach of children
TYLENOL with Codeineacetaminophen and codeine phosphate TABLET
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
TYLENOL with Codeineacetaminophen and codeine phosphate TABLET
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||