Vancomycin Hydrochloride
Vancomycin
FULL PRESCRIBING INFORMATION: CONTENTS*
- VANCOMYCIN HYDROCHLORIDE DESCRIPTION
- CLINICAL PHARMACOLOGY
- VANCOMYCIN HYDROCHLORIDE INDICATIONS AND USAGE
- VANCOMYCIN HYDROCHLORIDE CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- VANCOMYCIN HYDROCHLORIDE ADVERSE REACTIONS
- OVERDOSAGE
- VANCOMYCIN HYDROCHLORIDE DOSAGE AND ADMINISTRATION
- PREPARATION AND STABILITY
- INSTRUCTIONS FOR USE
- HOW SUPPLIED
- ANIMAL PHARMACOLOGY
- REFERENCES
- Principal Display Panel
- Principal Display Panel
FULL PRESCRIBING INFORMATION
Hydrochloride for Injection, USP
ADD-Vantage™ Vials
Rx only
To reduce the development of drug-resistant bacteria and maintain the effectiveness of vancomycin and other antibacterial drugs, vancomycin should be used only to treat or prevent infections that are proven or strongly suspected to be caused by bacteria.
VANCOMYCIN HYDROCHLORIDE DESCRIPTION
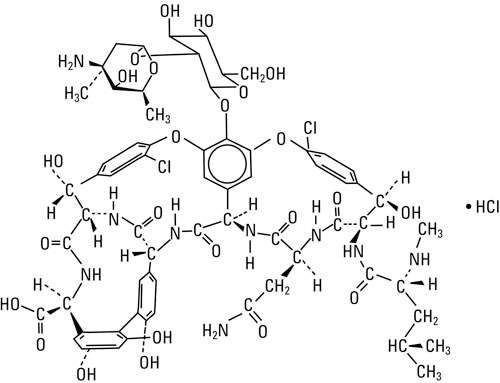
Vancomycin Hydrochloride for Injection, USP, intravenous, is a chromatographically purified tricyclic glycopeptide antibiotic derived from Amycolatopsis orientalis (formerly Nocardia orientalis ) and has the molecular formula C66H75Cl2N9O24 • HCl. The molecular weight is 1485.74; 500 mg of the base is equivalent to 0.34 mmol, 750 mg of the base is equivalent to 0.51 mmol, and 1 g of the base is equivalent to 0.67 mmol.
Vancomycin Hydrochloride has the following structural formula:
The ADD-Vantage™ vials contain sterile vancomycin hydrochloride equivalent to either 500 mg, 750 mg, or 1 g vancomycin activity for reconstitution in the ADD-Vantage flexible diluent container containing 5% dextrose injection or 0.9% sodium chloride injection. Vancomycin Hydrochloride is a white to tan lyophilized powder. May contain hydrochloric acid and/or sodium hydroxide for pH adjustment. When reconstituted in water, it forms a clear, light to dark tan solution with a pH of 4.0 (2.5 to 4.5). This product is oxygen sensitive.
The solutions contain no bacteriostat, antimicrobial agent (except vancomycin) or buffer and are intended for use only as a single-dose injection only with the ADD-Vantage Flexible Diluent Container.
FURTHER DILUTION IS REQUIRED BEFORE USE (see DOSAGE AND ADMINISTRATION ).
CLINICAL PHARMACOLOGY
Vancomycin is poorly absorbed after oral administration; it is given intravenously for therapy of systemic infections. Intramuscular injection is painful.
Vancomycin Hydrochloride for Injection, USP is administered intravenously for therapy of systemic infections.
In subjects with normal kidney function, multiple intravenous dosing of 1 g of vancomycin (15 mg/kg) infused over 60 minutes produces mean plasma concentrations of approximately 63 mcg/mL immediately after the completion of infusion, mean plasma concentrations of approximately 23 mcg/mL two hours after infusion, and mean plasma concentrations of approximately 8 mcg/mL eleven hours after the end of the infusion. Multiple dosing of 500 mg infused over 30 minutes produces mean plasma concentrations of about 49 mcg/mL at the completion of infusion, mean plasma concentrations of about 19 mcg/mL two hours after infusion, and mean plasma concentrations of about 10 mcg/mL six hours after infusion. The plasma concentrations during multiple dosing are similar to those after a single dose.
The mean elimination half-life of vancomycin from plasma is 4 to 6 hours in subjects with normal renal function. In the first 24 hours, about 75% of an administered dose of vancomycin is excreted in urine by glomerular filtration. Mean plasma clearance is about 0.058 L/kg/hr, and mean renal clearance is about 0.048 L/kg/hr. Renal dysfunction slows excretion of vancomycin. In anephric patients, the average half-life of elimination is 7.5 days. The distribution coefficient is from 0.3 to 0.43 L/kg. There is no apparent metabolism of the drug. About 60% of an intraperitoneal dose of vancomycin administered during peritoneal dialysis is absorbed systemically in six hours. Serum concentrations of about 10 mcg/mL are achieved by intraperitoneal injection of 30 mg/kg of vancomycin.
However, the safety and efficacy of the intraperitoneal use of vancomycin has not been established in adequate and well-controlled trials (see PRECAUTIONS ).
Total systemic and renal clearance of vancomycin may be reduced in the elderly.
Vancomycin is approximately 55% serum protein bound as measured by ultrafiltration at vancomycin serum concentrations of 10 to 100 mcg/mL. After I.V. administration of vancomycin hydrochloride, inhibitory concentrations are present in pleural, pericardial, ascitic, and synovial fluids; in urine; in peritoneal dialysis fluid; and in atrial appendage tissue. Vancomycin hydrochloride does not readily diffuse across normal meninges into the spinal fluid; but, when the meninges are inflamed, penetration into the spinal fluid occurs.
Microbiology
The bactericidal action of vancomycin results primarily from inhibition of cell-wall biosynthesis. In addition, vancomycin alters bacterial-cell-membrane permeability and RNA synthesis. There is no cross-resistance between vancomycin and other antibiotics. Vancomycin is not active in vitro against gram-negative bacilli, mycobacteria, or fungi.
Synergy
The combination of vancomycin and an aminoglycoside acts synergistically in vitro against many strains of Staphylococcus aureus , Streptococcus bovis , enterococci, and the viridans group streptococci.
Vancomycin has been shown to be active against most strains of the following microorganisms, both in vitro and in clinical infections as described in the INDICATIONS AND USAGE section.
Gram-positive bacteria
Diphtheroids
Enterococci (e.g., Enterococcus faecalis )
Staphylococci, including Staphylococcus aureus and Staphylococcus epidermidis (including heterogeneous methicillin-resistant strains) in adequate and well-controlled clinical trials.
Gram-positive bacteria
Listeria monocytogenes
Streptococcus pyogenes
Streptococcus pneumoniae (including penicillin-resistant strains)
Streptococcus agalactiae
Anaerobic Gram-positive bacteria
Actinomyces species
Lactobacillus species
Susceptibility Test Methods
When available, the clinical microbiology laboratory should provide the results of in vitro susceptibility test results for antimicrobial drugs used in local hospitals and practice areas to the physician as periodic reports that describe the susceptibility profile of nosocomial and community-acquired pathogens. These reports should aid the physician in selecting the most effective antimicrobial.
Dilution Techniques
Quantitative methods are used to determine antimicrobial minimum inhibitory concentrations (MIC's). These MIC's provide estimates of the susceptibility of bacteria to antimicrobial compounds. The MIC's should be determined using a standardized procedure. Standardized procedures are based on dilution method1,2 (broth, agar or microdilution) or equivalent using standardized inoculum and concentrations of vancomycin powder. The MIC values should be interpreted according to the criteria in Table 1.
Diffusion Techniques
Quantitative methods that require measurement of zone diameters also provide reproducible estimates of the susceptibility of bacteria to antimicrobial compounds. One such standardized procedure2,3 requires the use of standardized inoculum concentrations. This procedure uses paper disks impregnated with 30-mcg of vancomycin to test the susceptibility of microorganisms to vancomycin. Interpretation involves correlation of the diameter obtained in the disk test with the MIC for vancomycin.
Reports from the laboratory providing results of the standard single-disk susceptibility test with a 30-mcg vancomycin disk should be interpreted according to the following criteria in Table 1.
|
|
Minimum Inhibitory Concentrations |
Disk Diffusion Diameters |
||||
|
Pathogen |
Susceptible |
Intermediate |
Resistant |
Susceptible |
Intermediate |
Resistant |
|
Enterococci a |
≤4 |
8 – 16 |
≥32 |
≥17b |
15 – 16b |
≤14b |
|
Staphylococcus aureus |
≤2 |
4 – 8 |
≥16 |
–– |
–– |
–– |
|
Coagulase-negative staphylococci |
≤4 |
8 – 16 |
≥32 |
–– |
–– |
–– |
|
Streptococci other than S. pneumoniae |
≤1c,d |
–– |
–– |
≥17c,e |
–– |
–– |
|
a A ß-lactamase test using an inoculum ≥107 CFU/mL or direct colony growth and a nitrocefin-based substrate should be performed to detect either ampicillin or penicillin resistance due to ß-lactamase production. |
||||||
A report of “Susceptible” indicates that the pathogen is likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable. A report of “Intermediate” indicates that the result should be considered equivocal, and, if the microorganism is not fully susceptible to alternative, clinically feasible drugs, the test should be repeated. This category implies possible clinical applicability in body sites where the drug is physiologically concentrated or in situations where high dosage of drug can be used. This category also provides a buffer zone which prevents small uncontrolled technical factors from causing major discrepancies in interpretation. A report of “Resistant” indicates that the pathogen is not likely to be inhibited if the antimicrobial compound in the blood reaches the concentrations usually achievable; other therapy should be selected.
Quality Control
Standardized susceptibility test procedures require the use of laboratory control microorganisms to monitor and ensure the accuracy and precision of the supplies and reagents used in the assay, and the techniques of the individuals performing the test. Standard vancomycin powder should provide MIC values provided below. For the diffusion technique, the 30 mcg vancomycin disk should provide the following zone diameters with the quality control strains:
|
Organism (ATTC #) |
MIC range (mcg/mL) |
Disk diffusion range (mm) |
|
Enterococcus faecalis (29212) |
1 – 4 |
Not applicable |
|
Staphylococcus aureus (29213) |
0.5 – 2 |
Not applicable |
|
Staphylococcus aureus (25923) |
Not applicable |
17 – 21 |
|
Streptococcus pneumoniae (49619)a |
0.12 – 0.5 |
20 – 27 |
|
a Interpretative criteria applicable only to tests performed using cation-adjusted Mueller-Hinton broth with 2 to 5% lysed horse blood1. Disk diffusion interpretive criteria applicable only to tests performed using Mueller-Hinton agar with 5% defibrinated sheep blood and incubated in 5% CO2. |
||
VANCOMYCIN HYDROCHLORIDE INDICATIONS AND USAGE
Vancomycin hydrochloride is indicated for the treatment of serious or severe infections caused by susceptible strains of methicillin-resistant (beta-lactam-resistant) staphylococci. It is indicated for penicillin-allergic patients, for patients who cannot receive or who have failed to respond to other drugs, including the penicillins or cephalosporins, and for infections caused by vancomycin‑susceptible organisms that are resistant to other antimicrobial drugs. Vancomycin hydrochloride is indicated for initial therapy when methicillin-resistant staphylococci are suspected, but after susceptibility data are available, therapy should be adjusted accordingly.
Vancomycin hydrochloride is effective in the treatment of staphylococcal endocarditis. It’s effectiveness has been documented in other infections due to staphylococci, including septicemia, bone infections, lower respiratory tract infections, skin and skin-structure infections. When staphylococcal infections are localized and purulent, antibiotics are used as adjuncts to appropriate surgical measures.
Vancomycin hydrochloride has been reported to be effective alone or in combination with an aminoglycoside for endocarditis caused by Streptococcus viridans or S. bovis . For endocarditis caused by enterococci (e.g., E. faecalis ), vancomycin hydrochloride has been reported to be effective only in combination with an aminoglycoside.
Vancomycin hydrochloride has been reported to be effective for the treatment of diphtheroid endocarditis. Vancomycin hydrochloride has been used successfully in combination with either rifampin, an aminoglycoside, or both in early-onset prosthetic valve endocarditis caused by S. epidermidis or diphtheroids.
Specimens for bacteriologic cultures should be obtained in order to isolate and identify causative organisms and to determine their susceptibilities to vancomycin hydrochloride.
The parenteral form of vancomycin hydrochloride may be administered orally for treatment of antibiotic-associated pseudomembranous colitis produced by C. difficile and for staphylococcal enterocolitis. Parenteral administration of vancomycin hydrochloride alone is of unproven benefit for these indications. Vancomycin hydrochloride is not effective by the oral route for other types of infection.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of vancomycin and other antibacterial drugs, vancomycin should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
VANCOMYCIN HYDROCHLORIDE CONTRAINDICATIONS
Vancomycin Hydrochloride for Injection, USP is contraindicated in patients with known hypersensitivity to this antibiotic.
WARNINGS
Rapid bolus administration (e.g., over several minutes) may be associated with exaggerated hypotension, including shock and rarely cardiac arrest. Vancomycin hydrochloride should be administered in a dilute solution over a period of not less than 60 minutes to avoid rapid-infusion-related reactions. Stopping the infusion usually results in a prompt cessation of these reactions.
Ototoxicity has occurred in patients receiving vancomycin hydrochloride. It may be transient or permanent. It has been reported mostly in patients who have been given excessive doses, who have an underlying hearing loss, or who are receiving concomitant therapy with another ototoxic agent, such as an aminoglycoside. Vancomycin should be used with caution in patients with renal insufficiency because the risk of toxicity is appreciably increased by high, prolonged blood concentrations.
Dosage of vancomycin hydrochloride must be adjusted for patients with renal dysfunction (see PRECAUTIONS and DOSAGE AND ADMINISTRATION ).
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including Vancomycin Hydrochloride for Injection, USP, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile , and surgical evaluation should be instituted as clinically indicated.
PRECAUTIONS
General
Clinically significant serum concentrations have been reported in some patients who have taken multiple oral doses of vancomycin for active C. difficile -induced pseudomembranous colitis.
Prolonged use of vancomycin may result in the overgrowth of nonsusceptible microorganisms. Careful observation of the patient is essential. If superinfection occurs during therapy, appropriate measures should be taken. In rare instances, there have been reports of pseudomembranous colitis due to C. difficile developing in patients who receive intravenous vancomycin.
In order to minimize the risk of nephrotoxicity when treating patients with underlying renal dysfunction or patients receiving concomitant therapy with an aminoglycoside, serial monitoring of renal function should be performed and particular care should be taken in following appropriate dosing schedules (see DOSAGE AND ADMINISTRATION ).
Serial tests of auditory function may be helpful in order to minimize the risk of ototoxicity.
Reversible neutropenia has been reported in patients receiving vancomycin hydrochloride (see ADVERSE REACTIONS ). Patients who will undergo prolonged therapy with vancomycin hydrochloride or those who are receiving concomitant drugs which may cause neutropenia should have periodic monitoring of the leukocyte count.
Vancomycin hydrochloride is irritating to tissue and must be given by a secure intravenous route of administration. Pain, tenderness, and necrosis occur with intramuscular injection or with inadvertent extravasation. Thrombophlebitis may occur, the frequency and severity of which can be minimized by administering the drug slowly as a dilute solution (2.5 to 5 g/L) and by rotation of venous access sites.
There have been reports that the frequency of infusion-related events (including hypotension, flushing, erythema, urticaria, and pruritus) increases with the concomitant administration of anesthetic agents. Infusion-related events may be minimized by the administration of vancomycin hydrochloride as a 60-minute infusion prior to anesthetic induction.
The safety and efficacy of vancomycin administration by the intrathecal (intralumbar or intraventricular) route or by intraperitoneal route have not been established by adequate and well-controlled trials.
Reports have revealed that administration of Vancomycin Hydrochloride for Injection, USP by the intraperitoneal route during continuous ambulatory peritoneal dialysis (CAPD) has resulted in a syndrome of chemical peritonitis. To date, this syndrome has ranged from a cloudy dialysate alone to a cloudy dialysate accompanied by variable degrees of abdominal pain and fever. This syndrome appears to be short-lived after discontinuation of intraperitoneal vancomycin.
Prescribing vancomycin in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Information for Patients
Patients should be counseled that antibacterial drugs including vancomycin should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When vancomycin is prescribed to treat a bacterial infection, the patient should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by vancomycin or other antibacterial drugs in the future.
Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibiotic. If this occurs, patients should contact their physician as soon as possible.
Drug Interactions
Concomitant administration of vancomycin and anesthetic agents has been associated with erythema and histamine-like flushing (see Pediatric Use under PRECAUTIONS ) and anaphylactoid reactions (see ADVERSE REACTIONS ).
Concurrent and/or sequential systemic or topical use of other potentially neurotoxic and/or nephrotoxic drugs, such as amphotericin B, aminoglycosides, bacitracin, polymyxin B, colistin, viomycin, or cisplatin, when indicated, requires careful monitoring.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Although no long-term studies in animals have been performed to evaluate carcinogenic potential, no mutagenic potential of Vancomycin Hydrochloride for Injection, USP was found in standard laboratory tests. No definitive fertility studies have been performed.
Pregnancy
Teratogenic Effects
Category C
Animal reproduction studies have not been conducted with Vancomycin hydrochloride. It is not known whether Vancomycin hydrochloride can affect reproduction capacity. In a controlled clinical study, the potential ototoxic and nephrotoxic effects of Vancomycin hydrochloride on infants were evaluated when the drug was administered to pregnant women for serious staphylococcal infections complicating intravenous drug abuse. Vancomycin hydrochloride was found in cord blood. No sensorineural hearing loss or nephrotoxicity attributable to vancomycin was noted. One infant whose mother received vancomycin in the third trimester experienced conductive hearing loss that was not attributed to the administration of vancomycin. Because the number of patients treated in this study was limited and vancomycin was administered only in the second and third trimesters, it is not known whether vancomycin causes fetal harm. Vancomycin should be given to a pregnant woman only if clearly needed.
Nursing Mothers
Vancomycin is excreted in human milk. Caution should be exercised when vancomycin is administered to a nursing woman. Because of the potential for adverse events, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
In pediatric patients, it may be appropriate to confirm desired vancomycin serum concentrations. Concomitant administration of vancomycin and anesthetic agents has been associated with erythema and histamine-like flushing in pediatric patients (see ADVERSE REACTIONS ).
Geriatric Use
The natural decrement of glomerular filtration with increasing age may lead to elevated vancomycin serum concentrations if dosage is not adjusted. Vancomycin dosage schedules should be adjusted in elderly patients (see DOSAGE AND ADMINISTRATION ).
VANCOMYCIN HYDROCHLORIDE ADVERSE REACTIONS
Infusion-Related Events
During or soon after rapid infusion of vancomycin hydrochloride, patients may develop anaphylactoid reactions, including hypotension (see ANIMAL PHARMACOLOGY ), wheezing, dyspnea, urticaria, or pruritus. Rapid infusion may also cause flushing of the upper body (“red neck”) or pain and muscle spasm of the chest and back. These reactions usually resolve within 20 minutes but may persist for several hours. Such events are infrequent if vancomycin hydrochloride is given by a slow infusion over 60 minutes. In studies of normal volunteers, infusion-related events did not occur when vancomycin hydrochloride was administered at a rate of 10 mg/min or less.
Nephrotoxicity
Renal failure, principally manifested by increased serum creatinine or BUN concentrations, especially in patients given large doses of vancomycin, has been reported. Rare cases of interstitial nephritis have been reported. Most of these have occurred in patients who were given aminoglycosides concomitantly or who had preexisting kidney dysfunction. When vancomycin hydrochloride was discontinued, azotemia resolved in most patients.
Gastrointestinal
Onset of pseudomembranous colitis symptoms may occur during or after antibiotic treatment (see WARNINGS ).
Ototoxicity
A few dozen cases of hearing loss associated with vancomycin hydrochloride have been reported. Most of these patients had kidney dysfunction or a preexisting hearing loss, or were receiving concomitant treatment with an ototoxic drug. Vertigo, dizziness, and tinnitus have been reported rarely.
Hematopoietic
Reversible neutropenia, usually starting one week or more after onset of therapy with vancomycin hydrochloride or after a total dosage of more than 25 g, has been reported for several dozen patients. Neutropenia appears to be promptly reversible when vancomycin hydrochloride is discontinued. Thrombocytopenia has rarely been reported.
Although a causal relationship has not been established, reversible agranulocytosis (granulocytes <500/mm3) has been reported rarely.
Phlebitis
Inflammation at the injection site has been reported.
Miscellaneous
Infrequently, patients have been reported to have had anaphylaxis, drug fever, nausea, chills, eosinophilia, rashes (including exfoliative dermatitis), linear IgA bullous dermatosis, Stevens-Johnson syndrome, toxic epidermal necrolysis, and vasculitis in association with the administration of vancomycin.
Chemical peritonitis has been reported following intraperitoneal administration of vancomycin (see PRECAUTIONS ).
Post Marketing Reports
The following adverse reactions have been identified during post-approval use of vancomycin. Because these reactions are reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency or establish a causal relationship to the drug exposure.
Skin and Subcutaneous Tissue Disorders
Drug Rash with Eosinophilia and Systemic Symptoms (DRESS)
To report SUSPECTED ADVERSE EVENTS, contact FDA at 1-800-FDA-1088 or www.fda.gov.
OVERDOSAGE
Supportive care is advised, with maintenance of glomerular filtration. Vancomycin is poorly removed by dialysis. Hemofiltration and hemoperfusion with polysulfone resin have been reported to result in increased vancomycin clearance.
The median lethal intravenous dose is 319 mg/kg in rats and 400 mg/kg in mice.
To obtain up-to-date information about the treatment of overdose, a good resource is your certified Regional Poison Control Center. Telephone numbers of certified poison control centers are listed in the Physicians’ Desk Reference (PDR). In managing overdosage, consider the possibility of multiple drug overdoses, interaction among drugs, and unusual drug kinetics in your patient.
VANCOMYCIN HYDROCHLORIDE DOSAGE AND ADMINISTRATION
An infusion rate of 10 mg/min or less is associated with fewer infusion-related events (see ADVERSE REACTIONS ). Infusion-related events are related to both concentration and rate of administration of vancomycin. Concentrations of no more than 5 mg/mL and rates of no more than 10 mg/min are recommended in adults (see also age-specific recommendations).
In selected patients in need of fluid restriction, a concentration up to 10 mg/mL may be used; use of such higher concentrations may increase the risk of infusion-related events. Infusion-related events may occur, however, at any rate or concentration.
The use of ADD-Vantage vials of vancomycin hydrochloride is indicated only when doses of 500 mg, 750 mg or 1 g are appropriate. Patient factors, such as renal function and age, are critical in calculating correct dosage regimens (see below). If doses of 500 mg, 750 mg or 1 g are determined to be inappropriate, conventional vials of vancomycin hydrochloride should be used. ADD-VANTAGE VIALS OF VANCOMYCIN HYDROCHLORIDE SHOULD NOT BE USED IN NEONATES, INFANTS, OR PEDIATRIC PATIENTS WHO REQUIRE DOSES OF LESS THAN 500 MG.
Patients with Normal Renal Function
Adults
The usual daily intravenous dose is 2 g divided either as 500 mg every six hours or 1 g every 12 hours. Each dose should be administered at no more than 10 mg/min, or over a period of at least 60 minutes, whichever is longer. Other patient factors, such as age or obesity, may call for modification of the usual daily dose.
Pediatric Patients
The usual intravenous dosage of vancomycin hydrochloride is 10 mg/kg per dose given every six hours. Each dose should be administered over a period of at least 60 minutes. Close monitoring of serum concentrations of vancomycin is recommended in these patients.
Neonates
In pediatric patients up to the age of 1 month, the total daily intravenous dosage may be lower. In neonates, an initial dose of 15 mg/kg is suggested, followed by 10 mg/kg every 12 hours for neonates in the first week of life and every eight hours thereafter up to the age of one month. Each dose should be administered over 60 minutes. In premature infants, vancomycin clearance decreases as postconceptional age decreases. Therefore, longer dosing intervals may be necessary in premature infants. Close monitoring of serum concentrations of vancomycin is recommended in these patients.
Patients with Impaired Renal Function and Elderly Patients
Dosage adjustment must be made in patients with impaired renal function. In premature infants and in the elderly, greater dosage reductions than expected may be necessary because of decreased renal function. Measurement of vancomycin serum concentrations can be helpful in optimizing therapy, especially in seriously ill patients with changing renal function. Vancomycin serum concentrations can be determined by use of microbiologic assay, radioimmunoassay, fluorescence polarization immunoassay, fluorescence immunoassay, or high-pressure liquid chromatography.
If creatinine clearance can be measured or estimated accurately, the dosage for most patients with renal impairment can be calculated using the following table. The dosage of vancomycin hydrochloride per day in mg is about 15 times the glomerular filtration rate in mL/min:
|
Creatinine Clearance
|
Vancomycin Dose |
|
100 |
1,545 |
The initial dose should be no less than 15 mg/kg, even in patients with mild to moderate renal insufficiency.
The table is not valid for functionally anephric patients. For such patients, an initial dose of 15 mg/kg of body weight should be given to achieve prompt therapeutic serum concentrations. The dose required to maintain stable concentrations is 1.9 mg/kg/24 h. In patients with marked renal impairment, it may be more convenient to give maintenance doses of 250 to 1000 mg once every several days rather than administering the drug on a daily basis. In anuria, a dose of 1000 mg every 7 to 10 days has been recommended.
When only serum creatinine concentration is known, the following formula (based on sex, weight, and age of the patient) may be used to calculate creatinine clearance. Calculated creatinine clearances (mL/min) are only estimates. The creatinine clearance should be measured promptly.
Men: Weight (kg) x (140 - age in years)
72 x serum creatinine concentration (mg/dL)
Women: 0.85 x above value
The serum creatinine must represent a steady state of renal function. Otherwise, the estimated value for creatinine clearance is not valid. Such a calculated clearance is an overestimate of actual clearance in patients with conditions: (1) characterized by decreasing renal function, such as shock, severe heart failure, or oliguria; (2) in which a normal relationship between muscle mass and total body weight is not present, such as in obese patients or those with liver disease, edema, or ascites; and (3) accompanied by debilitation, malnutrition, or inactivity.
The safety and efficacy of vancomycin administration by the intrathecal (intralumbar or intraventricular) route have not been assessed.
Intermittent infusion is the recommended method of administration.
PREPARATION AND STABILITY
Vancomycin Hydrochloride ADD-Vantage vials should be used only with approved diluents (5% dextrose injection or 0.9% sodium chloride injection) (see INSTRUCTIONS FOR USE ).
Chemical Stability
It has been shown that after reconstitution, the admixture solution prepared in either dextrose injection or sodium chloride injection may be stored for 24 hours at room temperature or in a refrigerator for 14 days without significant loss of potency. However, this information is not intended to suggest that it is acceptable practice to administer such an admixture well after the time of preparation. Admixtures should be prepared as close to the time of administration as is reasonable.
Intermittent infusion is the recommended method of administration.
The 500 mg ADD-Vantage vial should be joined with at least a 100 mL ADD-Vantage flexible diluent container, the 750 mg and the 1 g ADD-Vantage vial should be joined only to a 250 mL ADD-Vantage flexible diluent container. The desired dose diluted in this manner should be administered by intravenous infusion over a period of at least 60 minutes.
Vancomycin solution has a low pH and may cause physical instability of other compounds.
Mixtures of solutions of vancomycin and beta-lactam antibiotics have been shown to be physically incompatible. The likelihood of precipitation increases with higher concentrations of vancomycin. It is recommended to adequately flush the intravenous lines between the administration of these antibiotics. It is also recommended to dilute solutions of vancomycin to 5 mg/mL or less.
Although intravitreal injection is not an approved route of administration for vancomycin, precipitation has been reported after intravitreal injection of vancomycin and ceftazidime for endophthalmitis using different syringes and needles. The precipitates dissolved gradually, with complete clearing of the vitreous cavity over two months and with improvement of visual acuity.
Prior to administration, parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution or container permits.
For Oral Administration
NOTE: For information only. ADD-Vantage Vials cannot be used to supply vancomycin for this purpose.
Oral vancomycin is used in treating antibiotic-associated pseudomembranous colitis caused by C. difficile and for staphylococcal enterocolitis. Vancomycin is not effective by the oral route for other types of infections. The usual adult total daily dosage is 500 mg to 2 g given in 3 or 4 divided doses for 7 to 10 days. The total daily dosage in pediatric patients is 40 mg/kg of body weight in 3 or 4 divided doses for 7 to 10 days. The total daily dosage should not exceed 2 g. The appropriate dose may be diluted in 1 oz of water and given to the patient to drink. Common flavoring syrups may be added to the solution to improve the taste for oral administration. The diluted material may be administered via nasogastric tube.
INSTRUCTIONS FOR USE
To Use Vial in ADD-Vantage Flexible Diluent Container
To Open:
Peel overwrap at corner and remove solution container. Some opacity of the plastic due to moisture absorption during the sterilization process may be observed. This is normal and does not affect the solution quality or safety. The opacity will diminish gradually.
To Assemble Vial and Flexible Diluent Container:
(Use Aseptic Technique)
1. Remove the protective covers from the top of the vial and the vial port on the diluent container as follows:
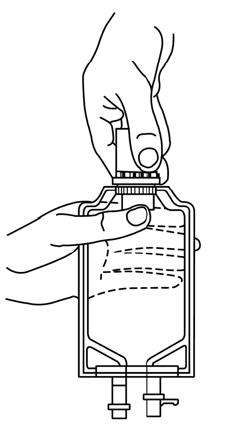
a. To remove the breakaway vial cap, swing the pull ring over the top of the vial and pull down far enough to start the opening (See Figure 1.), then pull straight up to remove the cap. (See Figure 2.) NOTE: Do not access vial with syringe.
|
Fig. 1 |
Fig. 2 |
|
|
|
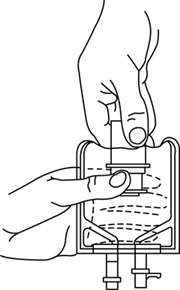
b. To remove the vial port cover, grasp the tab on the pull ring, pull up to break the tie membrane, then pull back to remove the cover. (See Figure 3.)
2. Screw the vial into the vial port until it will go no further. THE VIAL MUST BE SCREWED IN TIGHTLY TO ASSURE A SEAL. This occurs approximately 1/2 turn (180°) after the first audible click. (See Figure 4.) The clicking sound does not assure a seal; the vial must be turned as far as it will go. NOTE: Once vial is seated, do not attempt to remove. (See Figure 4.)
3. Recheck the vial to assure that it is tight by trying to turn it further in the direction of assembly.
4. Label appropriately.
|
Fig. 3 |
Fig. 4 |
|
|
|
To Reconstitute the Drug:
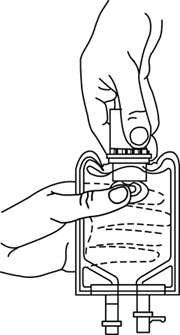
1. Squeeze the bottom of the diluent container gently to inflate the portion of the container surrounding the end of the drug vial.
2. With the other hand, push the drug vial down into the container telescoping the walls of the container. Grasp the inner cap of the vial through the walls of the container. (See Figure 5.)
3. Pull the inner cap from the drug vial. (See Figure 6.) Verify that the rubber stopper has been pulled out, allowing the drug and diluent to mix.
4. Mix container contents thoroughly and use within the specified time.
|
Fig. 5 |
Fig. 6 |
|
|
|
Preparation for Administration:
(Use Aseptic Technique)
1. Confirm the activation and admixture of vial contents.
2. Check for leaks by squeezing container firmly. If leaks are found, discard unit as sterility may be impaired.
3. Close flow control clamp of administration set.
4. Remove cover from outlet port at bottom of container.
5. Insert piercing pin of administration set into port with a twisting motion until the pin is firmly seated. NOTE: See full directions on administration set carton.
6. Lift the free end of the hanger loop on the bottom of the vial, breaking the two tie strings. Bend the loop outward to lock it in the upright position, then suspend container from hanger.
7. Squeeze and release drip chamber to establish proper fluid level in chamber.
8. Open flow control clamp and clear air from set. Close clamp.
9. Attach set to venipuncture device. If device is not indwelling, prime and make venipuncture.
10. Regulate rate of administration with flow control clamp.
WARNING: Do not use flexible containers in series connections.
HOW SUPPLIED
Vancomycin Hydrochloride for Injection, USP is supplied as a sterile powder in single-dose ADD-Vantage vials that contain either 500 mg, 750 mg or 1 g.
|
NDC Number
|
Fill
|
Units per Carton
|
|
0409-6534-01 |
500 mg |
10 ADD-Vantage™ Vials |
|
0409-6531-01 |
750 mg |
10 ADD-Vantage™ Vials |
|
0409-6535-01 |
1 g |
10 ADD-Vantage™ Vials |
Store at 20 to 25°C (68 to 77°F). [See USP Controlled Room Temperature.]
ANIMAL PHARMACOLOGY
In animal studies, hypotension and bradycardia occurred in dogs receiving an intravenous infusion of vancomycin, 25 mg/kg, at a concentration of 25 mg/mL and an infusion rate of 13.3 mL/min.
REFERENCES
- Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically; Approved Standard – 8th ed., CLSI document M07-A8. Clinical and Laboratory Standards Institute. Wayne, PA. January, 2009.
- Performance Standards for Antimicrobial Susceptibility Testing; 21st Informational Supplement, CLSI document M100-S21. Clinical and Laboratory Standards Institute. Wayne, PA. January, 2011.
- Performance Standards for Antimicrobial Disk Susceptibility Tests; Approved Standard – 10th ed., CLSI document M02-A10. Clinical and Laboratory Standards Institute. Wayne, PA. January, 2009.
- Moellering RC, Krogstad DJ, Greenblatt DJ: Vancomycin therapy in patients with impaired renal function: A nomogram for dosage. Ann Inter Med 1981;94:343.
Revised: 01/2012
EN-2970
Hospira, Inc., Lake Forest, IL 60045 USA
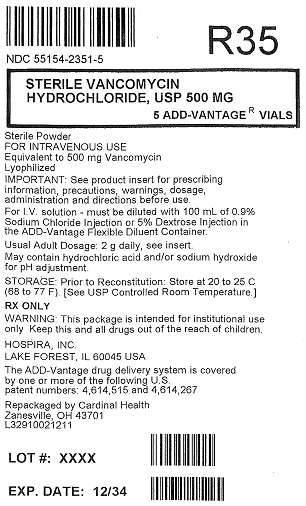
Principal Display Panel
NDC: 55154-2351-5
Sterile Vancomycin Hydrochloride, USP
500 mg
5 ADD-Vantage® Vials
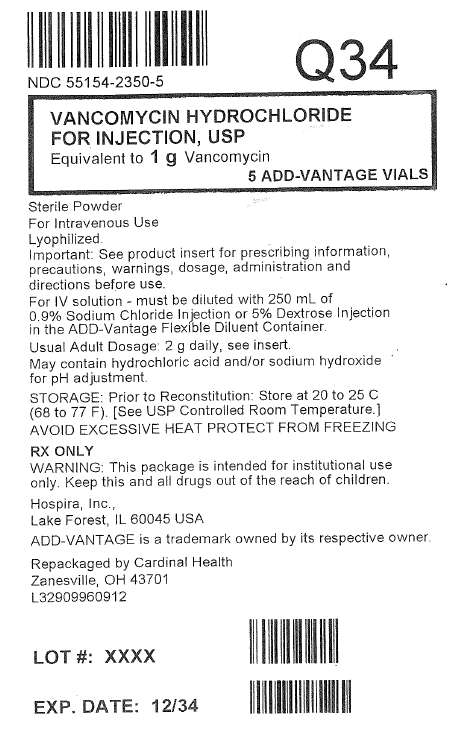
Principal Display Panel
NDC: 55154-2350-5
Vancomycin Hydrochloride for Injection, USP
Equivalent to 1g Vancomycin
5 ADD-Vantage Vials
Vancomycin HydrochlorideVANCOMYCIN HYDROCHLORIDE INJECTION, POWDER, LYOPHILIZED, FOR SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Vancomycin HydrochlorideVANCOMYCIN HYDROCHLORIDE INJECTION, POWDER, LYOPHILIZED, FOR SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||