Vimpat
Kremers Urban Pharmaceuticals Inc
HIGHLIGHTS OF PRESCRIBING INFORMATIONThese highlights do not include all the information needed to use VIMPAT safely and effectively. See full prescribing information for VIMPAT. VIMPAT (lacosamide) Tablet, Film Coated for Oral use, CV VIMPAT (lacosamide) Injection for Intravenous use, CV VIMPAT (lacosamide) Oral Solution, CVInitial U.S. Approval: 2008 RECENT MAJOR CHANGES Dosage and Administration (2.1) 01/2014 Dosage and Administration (2.2, 2.3) 09/2013 Warnings and Precautions (5.3) 09/2013 INDICATIONS AND USAGEVIMPAT is indicated for: partial-onset seizures (1.1): Tablets and oral solution are indicated for adjunctive therapy in patients ≥17 years. Injection is indicated as short term replacement when oral administration is not feasible in these patients. DOSAGE AND ADMINISTRATION Partial-onset seizures (2.1): Initially, give 50 mg twice daily (100 mg/day). Based on individual patient response and tolerability, the dose can be increased at weekly intervals by 100 mg per day given as two divided doses . The recommended maintenance dose is 200 mg to 400 mg per day given as two divided doses. VIMPAT injection may be given without further dilution or mixed in compatible diluent and should be administered intravenously over a period of 30 minutes to 60 minutes. (2.1) Oral-Intravenous Replacement therapy (2.1): When switching from oral VIMPAT, the initial total daily intravenous dosage of VIMPAT should be equivalent to the total daily dosage and frequency of oral VIMPAT. At the end of the intravenous treatment period, the patient may be switched to VIMPAT oral administration at the equivalent daily dosage and frequency of the intravenous administration. See full prescribing information for compatibility and stability (2.1) and dosing in patients with renal impairment (2.2) and hepatic impairment (2.3) . DOSAGE FORMS AND STRENGTHS 50 mg (pink), 100 mg (dark yellow), 150 mg (salmon), 200 mg (blue) film-coated tablets (3) 200 mg/20 mL single-use vial for intravenous use (3) 10 mg/mL oral solution (3) CONTRAINDICATIONS None WARNINGS AND PRECAUTIONS Suicidal Behavior and Ideation (5.1) Patients should be advised that VIMPAT may cause dizziness and ataxia. (5.2) Caution is advised for patients with known cardiac conduction problems [e.g., second-degree atrioventricular (AV) block], who are taking drugs known to induce PR interval prolongation, or with severe cardiac disease such as myocardial ischemia or heart failure. (5.3) Patients should be advised that VIMPAT may cause syncope. (5.4) In patients with seizure disorders, VIMPAT should be gradually withdrawn to minimize the potential of increased seizure frequency. (5.5) Multiorgan Hypersensitivity Reactions (5.6) Phenylketonurics (5.7) Side EffectsMost common adverse reactions (≥10% and greater than placebo) are diplopia, headache, dizziness, nausea (6.1) To report SUSPECTED ADVERSE REACTIONS, contact UCB, Inc. at 1-800-477-7877 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch USE IN SPECIFIC POPULATIONS To enroll in the UCB AED Pregnancy Registry call 1-888-537-7734 (toll free). To enroll in the North American Antiepileptic Drug Pregnancy Registry call 1-888-233-2334 (toll free). (8.1) Renal impairment: Dose adjustment is recommended for patients with severe renal impairment (creatinine clearance ≤ 30 mL/min). Dose supplementation should be considered following hemodialysis. (12.3) Hepatic impairment: Dose adjustment is recommended for patients with mild or moderate hepatic impairment. Use in severe hepatic impairment patients is not recommended. Patients with co-existing hepatic and renal impairment should be monitored closely during dose titration. (12.3)
FULL PRESCRIBING INFORMATION: CONTENTS*
- 1 VIMPAT INDICATIONS AND USAGE
- 2 VIMPAT DOSAGE AND ADMINISTRATION
- 3 DOSAGE FORMS AND STRENGTHS
- 4 VIMPAT CONTRAINDICATIONS
- 5 WARNINGS AND PRECAUTIONS
- 6 VIMPAT ADVERSE REACTIONS
- 7 DRUG INTERACTIONS
- 8 USE IN SPECIFIC POPULATIONS
- 9 DRUG ABUSE AND DEPENDENCE
- 10 OVERDOSAGE
- 11 VIMPAT DESCRIPTION
- 12 CLINICAL PHARMACOLOGY
- 13 NONCLINICAL TOXICOLOGY
- 14 CLINICAL STUDIES
- 16 HOW SUPPLIED/STORAGE AND HANDLING
- 17 PATIENT COUNSELING INFORMATION
- Medication Guide
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
1.1 Partial-Onset Seizures
VIMPAT (lacosamide) tablets and oral solution are indicated as adjunctive therapy in the treatment of partial-onset seizures in patients with epilepsy aged 17 years and older.
VIMPAT (lacosamide) injection for intravenous use is indicated as adjunctive therapy in the treatment of partial-onset seizures in patients with epilepsy aged 17 years and older when oral administration is temporarily not feasible.
2 DOSAGE AND ADMINISTRATION
VIMPAT may be taken with or without food.
When using VIMPAT oral solution, it is recommended that a calibrated measuring device be obtained and used. A household teaspoon or tablespoon is not an adequate measuring device. Healthcare providers should recommend a device that can measure and deliver the prescribed dose accurately, and provide instructions for measuring the dosage.
2.1 Partial-Onset Seizures
VIMPAT can be initiated with either oral or intravenous administration. The initial dose should be 50 mg twice daily (100 mg per day). Based on individual patient response and tolerability, the dose can be increased at weekly intervals by 100 mg per day given as two divided doses. The recommended maintenance dose is 200 mg to 400 mg/day, given as two divided doses. In clinical trials, the 600 mg daily dose was not more effective than the 400 mg daily dose, and was associated with a substantially higher rate of adverse reactions. [See Clinical Studies (14.1) ]
A gradual withdrawal of VIMPAT over at least 1 week is recommended. [See Withdrawal of Antiepileptic Drugs (5.5) ]
Switching from Oral to Intravenous Dosing
When switching from oral VIMPAT, the initial total daily intravenous dosage of VIMPAT should be equivalent to the total daily dosage and frequency of oral VIMPAT and should be infused intravenously over a period of 30 minutes to 60 minutes. There is experience with twice daily intravenous infusion for up to 5 days.
Switching from Intravenous to Oral Dosing
At the end of the intravenous treatment period, the patient may be switched to VIMPAT oral administration at the equivalent daily dosage and frequency of the intravenous administration.
Compatibility and Stability
VIMPAT injection can be administered intravenously without further dilution or may be mixed with diluents. VIMPAT injection was found to be physically compatible and chemically stable when mixed with the following diluents for at least 24 hours and stored in glass or polyvinyl chloride (PVC) bags at ambient room temperature 15°C to 30°C (59°F to 86°F).
Diluents:
Sodium Chloride Injection 0.9% (w/v)
Dextrose Injection 5% (w/v)
Lactated Ringer's Injection
The stability of VIMPAT injection in other infusion solutions has not been evaluated. Product with particulate matter or discoloration should not be used.
Any unused portion of VIMPAT injection should be discarded.
2.2 Patients with Renal Impairment
No dose adjustment is necessary in patients with mild to moderate renal impairment. A maximum dose of 300 mg per day VIMPAT is recommended for patients with severe renal impairment [creatinine clearance (CLCR) less than or equal to 30 mL/min] and in patients with endstage renal disease. VIMPAT is effectively removed from plasma by hemodialysis. Following a 4-hour hemodialysis treatment, dosage supplementation of up to 50% should be considered. In all renally impaired patients, the dose titration should be performed with caution. Patients with renal impairment who are taking strong inhibitors of CYP3A4 and CYP2C9 may have a significant increase in exposure to VIMPAT. Dose reduction may be necessary in these patients. [See Use in Specific Populations (8.6) and Clinical Pharmacology (12.3) ]
2.3 Patients with Hepatic Impairment
The dose titration should be performed with caution in patients with hepatic impairment. A maximum dose of 300 mg per day is recommended for patients with mild or moderate hepatic impairment.
VIMPAT use is not recommended in patients with severe hepatic impairment. Patients with hepatic impairment who are taking strong inhibitors of CYP3A4 and CYP2C9 may have a significant increase in exposure to VIMPAT. Dose reduction may be necessary in these patients. [See Use in Specific Populations (8.7) and Clinical Pharmacology (12.3) ]
3 DOSAGE FORMS AND STRENGTHS
50 mg (pink), 100 mg (dark yellow), 150 mg (salmon), and 200 mg (blue) film-coated tablets
200 mg/20 mL injection
10 mg/mL oral solution
4 CONTRAINDICATIONS
None.
5 WARNINGS AND PRECAUTIONS
5.1 Suicidal Behavior and Ideation
Antiepileptic drugs (AEDs), including VIMPAT, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number of events is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5-100 years) in the clinical trials analyzed.
Table 1 shows absolute and relative risk by indication for all evaluated AEDs.
| Indication | Placebo Patients with Events Per 1000 Patients |
Drug Patients with Events Per 1000 Patients |
Relative Risk: Incidence of Events in Drug Patients/Incidence in Placebo Patients |
Risk Difference: Additional Drug Patients with Events Per 1000 Patients |
|---|---|---|---|---|
| Epilepsy | 1.0 | 3.4 | 3.5 | 2.4 |
| Psychiatric | 5.7 | 8.5 | 1.5 | 2.9 |
| Other | 1.0 | 1.8 | 1.9 | 0.9 |
| Total | 2.4 | 4.3 | 1.8 | 1.9 |
The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar.
Anyone considering prescribing VIMPAT or any other AED must balance this risk with the risk of untreated illness. Epilepsy and many other illnesses for which antiepileptics are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
Patients, their caregivers, and families should be informed that AEDs increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
5.2 Dizziness and Ataxia
Patients should be advised that VIMPAT may cause dizziness and ataxia. Accordingly, they should be advised not to drive a car or to operate other complex machinery until they are familiar with the effects of VIMPAT on their ability to perform such activities.
In patients with partial-onset seizures taking 1 to 3 concomitant AEDs, dizziness was experienced by 25% of patients randomized to the recommended doses (200 to 400 mg/day) of VIMPAT (compared with 8% of placebo patients) and was the adverse event most frequently leading to discontinuation (3%). Ataxia was experienced by 6% of patients randomized to the recommended doses (200 to 400 mg/day) of VIMPAT (compared to 2% of placebo patients). The onset of dizziness and ataxia was most commonly observed during titration. There was a substantial increase in these adverse events at doses higher than 400 mg/day. [See Adverse Reactions/Table 2 (6.1) ]
5.3 Cardiac Rhythm and Conduction Abnormalities
Dose-dependent prolongations in PR interval with VIMPAT have been observed in clinical studies in patients and in healthy volunteers. [See Clinical Pharmacology (12.2) ] In clinical trials in patients with partial-onset epilepsy, asymptomatic first-degree atrioventricular (AV) block was observed as an adverse reaction in 0.4% (4/944) of patients randomized to receive VIMPAT and 0% (0/364) of patients randomized to receive placebo. In clinical trials in patients with diabetic neuropathy, asymptomatic first-degree AV block was observed as an adverse reaction in 0.5% (5/1023) of patients receiving VIMPAT and 0% (0/291) of patients receiving placebo. Second degree and complete AV block have been reported inpatients in pain studies and in patients with seizures. When VIMPAT is given with other drugs that prolong the PR interval, further PR prolongation is possible.
VIMPAT should be used with caution in patients with known conduction problems (e.g. marked first-degree AV block, second-degree or higher AV block and sick sinus syndrome without pacemaker, sodium channelopathies (e.g., Brugada Syndrome), on concomitant medications that prolong PR interval, or with severe cardiac disease such as myocardial ischemia or heart failure, or structural heart disease. In such patients, obtaining an ECG before beginning VIMPAT, and after VIMPAT is titrated to steady-state, is recommended.
In the short-term investigational trials of VIMPAT in epilepsy patients, there were no cases of atrial fibrillation or flutter. Both atrial fibrillation and atrial flutter have been reported in open label epilepsy trials and in postmarketing experience. In patients with diabetic neuropathy, 0.5% of patients treated with VIMPAT experienced an adverse reaction of atrial fibrillation or atrial flutter, compared to 0% of placebo-treated patients. VIMPAT administration may predispose to atrial arrhythmias (atrial fibrillation or flutter), especially in patients with diabetic neuropathy and/or cardiovascular disease.
5.4 Syncope
In the short-term controlled trials of VIMPAT in epilepsy patients with no significant system illnesses, there was no increase in syncope compared to placebo. In the short-term controlled trials of VIMPAT in patients with diabetic neuropathy, 1.2% of patients who were treated with VIMPAT reported an adverse reaction of syncope or loss of consciousness, compared to 0% of placebo-treated patients with diabetic neuropathy. Most of the cases of syncope were observed in patients receiving doses above 400 mg/day. The cause of syncope was not determined in most cases. However, several were associated with either changes in orthostatic blood pressure, atrial flutter/fibrillation (and associated tachycardia), or bradycardia.
5.5 Withdrawal of Antiepileptic Drugs (AEDs)
As with all AEDs, VIMPAT should be withdrawn gradually (over a minimum of 1 week) to minimize the potential of increased seizure frequency in patients with seizure disorders.
5.6 Multiorgan Hypersensitivity Reactions
One case of symptomatic hepatitis and nephritis was observed among 4011 subjects exposed to VIMPAT during clinical development. The event occurred in a healthy volunteer, 10 days after stopping VIMPAT treatment. The subject was not taking any concomitant medication and potential known viral etiologies for hepatitis were ruled out. The subject fully recovered within a month, without specific treatment. The case is consistent with a delayed multiorgan hypersensitivity reaction. Additional potential cases included 2 with rash and elevated liver enzymes and 1 with myocarditis and hepatitis of uncertain etiology.
Multiorgan hypersensitivity reactions (also known as Drug Reaction with Eosinophilia and Systemic Symptoms, or DRESS) have been reported with other anticonvulsants and typically, although not exclusively, present with fever and rash associated with other organ system involvement, that may or may not include eosinophilia, hepatitis, nephritis, lymphadenopathy, and/or myocarditis. Because this disorder is variable in its expression, other organ system signs and symptoms not noted here may occur. If this reaction is suspected, VIMPAT should be discontinued and alternative treatment started.
5.7 Phenylketonurics
VIMPAT oral solution contains aspartame, a source of phenylalanine. A 200 mg dose of VIMPAT oral solution (equivalent to 20 mL) contains 0.32 mg of phenylalanine.
6 ADVERSE REACTIONS
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In all controlled and uncontrolled trials in patients with partial-onset seizures, 1327 patients have received VIMPAT of whom 1000 have been treated for longer than 6 months and 852 for longer than 12 months.
6.1 Clinical Trials Experience
Controlled Trials
Adverse reactions leading to discontinuation
In controlled clinical trials, the rate of discontinuation as a result of an adverse event was 8% and 17% in patients randomized to receive VIMPAT at the recommended doses of 200 and 400 mg/day, respectively, 29% at 600 mg/day, and 5% in patients randomized to receive placebo. The adverse events most commonly (>1% in the VIMPAT total group and greater than placebo) leading to discontinuation were dizziness, ataxia, vomiting, diplopia, nausea, vertigo, and vision blurred.
Most common adverse reactions
Table 2 gives the incidence of treatment-emergent adverse events that occurred in ≥2% of adult patients with partial-onset seizures in the total VIMPAT group and for which the incidence was greater than placebo. The majority of adverse events in the VIMPAT patients were reported with a maximum intensity of 'mild' or 'moderate'.
|
System Organ Class/ Preferred Term |
Placebo N=364 % |
VIMPAT 200 mg/day N=270 % |
VIMPAT 400 mg/day N=471 % |
VIMPAT 600 mg/day N=203 % |
VIMPAT Total N=944 % |
| Ear and labyrinth disorder | |||||
| Vertigo | 1 | 5 | 3 | 4 | 4 |
| Eye disorders | |||||
| Diplopia | 2 | 6 | 10 | 16 | 11 |
| Vision blurred | 3 | 2 | 9 | 16 | 8 |
| Gastrointestinal disorders | |||||
| Nausea | 4 | 7 | 11 | 17 | 11 |
| Vomiting | 3 | 6 | 9 | 16 | 9 |
| Diarrhea | 3 | 3 | 5 | 4 | 4 |
| General disorders and administration site conditions | |||||
| Fatigue | 6 | 7 | 7 | 15 | 9 |
| Gait disturbance | <1 | <1 | 2 | 4 | 2 |
| Asthenia | 1 | 2 | 2 | 4 | 2 |
| Injury, poisoning and procedural complications | |||||
| Contusion | 3 | 3 | 4 | 2 | 3 |
| Skin laceration | 2 | 2 | 3 | 3 | 3 |
| Nervous system disorders | |||||
| Dizziness | 8 | 16 | 30 | 53 | 31 |
| Headache | 9 | 11 | 14 | 12 | 13 |
| Ataxia | 2 | 4 | 7 | 15 | 8 |
| Somnolence | 5 | 5 | 8 | 8 | 7 |
| Tremor | 4 | 4 | 6 | 12 | 7 |
| Nystagmus | 4 | 2 | 5 | 10 | 5 |
| Balance disorder | 0 | 1 | 5 | 6 | 4 |
| Memory impairment | 2 | 1 | 2 | 6 | 2 |
| Psychiatric disorders | |||||
| Depression | 1 | 2 | 2 | 2 | 2 |
| Skin and subcutaneous disorders | |||||
| Pruritus | 1 | 3 | 2 | 3 | 2 |
Laboratory abnormalities
Abnormalities in liver function tests have been observed in controlled trials with VIMPAT in adult patients with partial-onset seizures who were taking 1 to 3 concomitant anti-epileptic drugs. Elevations of ALT to ≥3× ULN occurred in 0.7% (7/935) of VIMPAT patients and 0% (0/356) of placebo patients. One case of hepatitis with transaminases >20x ULN was observed in one healthy subject 10 days after VIMPAT treatment completion, along with nephritis (proteinuria and urine casts). Serologic studies were negative for viral hepatitis. Transaminases returned to normal within one month without specific treatment. At the time of this event, bilirubin was normal. The hepatitis/nephritis was interpreted as a delayed hypersensitivity reaction to VIMPAT.
Other Side Effects in Patients with Partial-Onset Seizures
The following is a list of treatment-emergent adverse events reported by patients treated with VIMPAT in all clinical trials in patients with partial-onset seizures, including controlled trials and long-term open-label extension trials. Events addressed in other tables or sections are not listed here. Events included in this list from the controlled trials occurred more frequently on drug than on placebo and were based on consideration of VIMPAT pharmacology, frequency above that expected in the population, seriousness, and likelihood of a relationship to VIMPAT. Events are further classified within system organ class.
Blood and lymphatic system disorders: neutropenia, anemia
Cardiac disorders: palpitations
Ear and labyrinth disorders: tinnitus
Gastrointestinal disorders: constipation, dyspepsia, dry mouth, oral hypoaesthesia
General disorders and administration site conditions: irritability, pyrexia, feeling drunk
Injury, poisoning, and procedural complications: fall
Musculoskeletal and connective tissue disorders: muscle spasms
Nervous system disorders: paresthesia, cognitive disorder, hypoaesthesia, dysarthria, disturbance in attention, cerebellar syndrome
Psychiatric disorders: confusional state, mood altered, depressed mood
Intravenous Side Effects
Adverse reactions with intravenous administration generally appeared similar to those observed with the oral formulation, although intravenous administration was associated with local adverse events such as injection site pain or discomfort (2.5%), irritation (1%), and erythema (0.5%). One case of profound bradycardia (26 bpm: BP 100/60 mmHg) was observed in a patient during a 15 minute infusion of 150 mg VIMPAT. This patient was on a beta-blocker. Infusion was discontinued and the patient experienced a rapid recovery.
Comparison of Gender and Race
The overall adverse event rate was similar in male and female patients. Although there were few non-Caucasian patients, no differences in the incidences of adverse events compared to Caucasian patients were observed.
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of VIMPAT. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Blood and lymphatic system disorders: Agranulocytosis
Cardiac disorders: Bradycardia
Psychiatric disorders: Aggression, agitation, hallucination, insomnia, psychotic disorder
Skin and subcutaneous tissue disorders: Angioedema, rash, urticaria, Stevens-Johnson syndrome, toxic epidermal necrolysis
7 DRUG INTERACTIONS
Drug-drug interaction studies in healthy subjects showed no pharmacokinetic interactions between VIMPAT and carbamazepine, valproate, digoxin, metformin, omeprazole, midazolam, or an oral contraceptive containing ethinylestradiol and levonorgestrel. There was no evidence for any relevant drug-drug interaction of VIMPAT with common AEDs in the placebo-controlled clinical trials in patients with partial-onset seizures. [See Clinical Pharmacology (12.3) ]
The lack of pharmacokinetic interaction does not rule out the possibility of pharmacodynamic interactions, particularly among drugs that affect the heart conduction system.
Patients with renal or hepatic impairment who are taking strong inhibitors of CYP3A4 and CYP2C9 may have a significant increase in exposure to VIMPAT. Dose reduction may be necessary in these patients.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Pregnancy Category C
Lacosamide produced developmental toxicity (increased embryofetal and perinatal mortality, growth deficit) in rats following administration during pregnancy. Developmental neurotoxicity was observed in rats following administration during a period of postnatal development corresponding to the third trimester of human pregnancy. These effects were observed at doses associated with clinically relevant plasma exposures.
Lacosamide has been shown in vitro to interfere with the activity of collapsin response mediator protein-2 (CRMP-2), a protein involved in neuronal differentiation and control of axonal outgrowth. Potential related adverse effects on CNS development cannot be ruled out.
There are no adequate and well-controlled studies in pregnant women. VIMPAT should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Oral administration of lacosamide to pregnant rats (20, 75, or 200 mg/kg/day) and rabbits (6.25, 12.5, or 25 mg/kg/day) during the period of organogenesis did not produce any teratogenic effects. However, the maximum doses evaluated were limited by maternal toxicity in both species and embryofetal death in rats. These doses were associated with maternal plasma lacosamide exposures [area under the plasma-time concentration curve; (AUC)] ≈2 and 1 times (rat and rabbit, respectively) that in humans at the maximum recommended human dose (MRHD) of 400 mg/day.
When lacosamide (25, 70, or 200 mg/kg/day) was orally administered to rats throughout gestation, parturition, and lactation, increased perinatal mortality and decreased body weights were observed in the offspring at the highest dose. The no-effect dose for pre- and post-natal developmental toxicity in rats (70 mg/kg/day) was associated with a maternal plasma lacosamide AUC approximately equal to that in humans at the MRHD.
Oral administration of lacosamide (30, 90, or 180 mg/kg/day) to rats during the neonatal and juvenile periods of postnatal development resulted in decreased brain weights and long-term neurobehavioral changes (altered open field performance, deficits in learning and memory). The early postnatal period in rats is generally thought to correspond to late pregnancy in humans in terms of brain development. The no-effect dose for developmental neurotoxicity in rats was associated with a plasma lacosamide AUC approximately 0.5 times that in humans at the MRHD.
Pregnancy Registry
UCB, Inc. has established the UCB AED Pregnancy Registry to advance scientific knowledge about safety and outcomes in pregnant women being treated with VIMPAT. To ensure broad program access and reach, either a healthcare provider or the patient can initiate enrollment in the UCB AED Pregnancy Registry by calling 1-888-537-7734 (toll free).
Physicians are also advised to recommend that pregnant patients taking VIMPAT enroll in the North American Antiepileptic Drug Pregnancy Registry. This can be done by calling the toll free number 1-888-233-2334, and must be done by patients themselves. Information on the registry can also be found at the website http://www.aedpregnancyregistry.org/.
8.2 Labor and Delivery
The effects of VIMPAT on labor and delivery in pregnant women are unknown. In a pre- and post-natal study in rats, there was a tendency for prolonged gestation in all lacosamide treated groups at plasma exposures (AUC) at or below the plasma AUC in humans at the maximum recommended human dose of 400 mg/day.
8.3 Nursing Mothers
Studies in lactating rats have shown that lacosamide and/or its metabolites are excreted in milk. It is not known whether VIMPAT is excreted in human milk. Because many drugs are excreted into human milk, a decision should be made whether to discontinue nursing or to discontinue VIMPAT, taking into account the importance of the drug to the mother.
8.4 Pediatric Use
The safety and effectiveness of VIMPAT in pediatric patients <17 years have not been established.
Lacosamide has been shown in vitro to interfere with the activity of collapsin response mediator protein-2 (CRMP-2), a protein involved in neuronal differentiation and control of axonal outgrowth. Potential related adverse effects on CNS development cannot be ruled out. Administration of lacosamide to rats during the neonatal and juvenile periods of postnatal development resulted in decreased brain weights and long-term neurobehavioral changes (altered open field performance, deficits in learning and memory). The no-effect dose for developmental neurotoxicity in rats was associated with a plasma lacosamide exposure (AUC) approximately 0.5 times the human plasma AUC at the maximum recommended human dose of 400 mg/day.
8.5 Geriatric Use
There were insufficient numbers of elderly patients enrolled in partial-onset seizure trials (n=18) to adequately assess the effectiveness of VIMPAT in this population.
No VIMPAT dose adjustment based on age is considered necessary. In elderly patients, dose titration should be performed with caution. [See Dosage and Administration (2.2) and Clinical Pharmacology (12.3) ]
8.6 Patients with Renal Impairment
A maximum dose of 300 mg/day is recommended for patients with severe renal impairment (CLCR≤30 mL/min) and in patients with endstage renal disease. VIMPAT is effectively removed from plasma by hemodialysis. Dosage supplementation of up to 50% following hemodialysis should be considered. In all renally impaired patients, dose titration should be performed with caution. [See Dosage and Administration (2.2) and Clinical Pharmacology (12.3) ]
8.7 Patients with Hepatic Impairment
Patients with mild to moderate hepatic impairment should be observed closely during dose titration. A maximum dose of 300 mg/day is recommended for patients with mild to moderate hepatic impairment. The pharmacokinetics of lacosamide has not been evaluated in severe hepatic impairment. VIMPAT use is not recommended in patients with severe hepatic impairment. [See Dosage and Administration (2.3) and Clinical Pharmacology (12.3) ] Patients with co-existing hepatic and renal impairment should be monitored closely during dose titration.
9 DRUG ABUSE AND DEPENDENCE
9.1 Controlled Substance
VIMPAT is a Schedule V controlled substance.
9.2 Abuse
In a human abuse potential study, single doses of 200 mg and 800 mg lacosamide produced euphoria-type subjective responses that differentiated statistically from placebo; at 800 mg, these euphoria-type responses were statistically indistinguishable from those produced by alprazolam, a Schedule IV drug. The duration of the euphoria-type responses following lacosamide was less than that following alprazolam. A high rate of euphoria was also reported as an adverse event in the human abuse potential study following single doses of 800 mg lacosamide (15% [5/34]) compared to placebo (0%) and in two pharmacokinetic studies following single and multiple doses of 300-800 mg lacosamide (ranging from 6% [2/33] to 25% [3/12]) compared to placebo (0%). However, the rate of euphoria reported as an adverse event in the VIMPAT development program at therapeutic doses was less than 1%.
9.3 Dependence
Abrupt termination of lacosamide in clinical trials with diabetic neuropathic pain patients produced no signs or symptoms that are associated with a withdrawal syndrome indicative of physical dependence. However, psychological dependence cannot be excluded due to the ability of lacosamide to produce euphoria-type adverse events in humans.
10 OVERDOSAGE
10.1 Signs, Symptoms, and Laboratory Findings of Acute Overdose in Humans
There is limited clinical experience with VIMPAT overdose in humans. The highest reported accidental overdose of VIMPAT during clinical development was 1200 mg/day which was non-fatal. The types of adverse events experienced by patients exposed to supratherapeutic doses during the trials were not clinically different from those of patients administered recommended doses of VIMPAT.
There has been a single case of intentional overdose by a patient who self-administered 12 grams VIMPAT along with large doses of zonisamide, topiramate, and gabapentin. The patient presented in a coma and was hospitalized. An EEG revealed epileptic waveforms. The patient recovered 2 days later.
10.2 Treatment or Management of Overdose
There is no specific antidote for overdose with VIMPAT. Standard decontamination procedures should be followed. General supportive care of the patient is indicated including monitoring of vital signs and observation of the clinical status of patient. A Certified Poison Control Center should be contacted for up to date information on the management of overdose with VIMPAT.
Standard hemodialysis procedures result in significant clearance of VIMPAT (reduction of systemic exposure by 50% in 4 hours). Hemodialysis has not been performed in the few known cases of overdose, but may be indicated based on the patient's clinical state or in patients with significant renal impairment.
11 DESCRIPTION
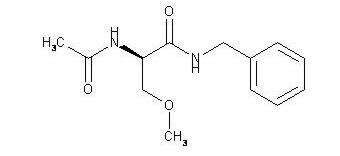
The chemical name of lacosamide, the single (R)-enantiomer, is (R)-2-acetamido-N-benzyl-3-methoxypropionamide (IUPAC). Lacosamide is a functionalized amino acid. Its molecular formula is C13H18N2O3 and its molecular weight is 250.30. The chemical structure is:
Lacosamide is a white to light yellow powder. It is sparingly soluble in water and slightly soluble in acetonitrile and ethanol.
11.1 VIMPAT Tablets
VIMPAT tablets contain the following inactive ingredients: colloidal silicon dioxide, crospovidone, hydroxypropylcellulose, hypromellose, magnesium stearate, microcrystalline cellulose, polyethylene glycol, polyvinyl alcohol, talc, titanium dioxide, and dye pigments as specified below:
VIMPAT tablets are supplied as debossed tablets and contain the following coloring agents:
50 mg tablets: red iron oxide, black iron oxide, FD&C Blue #2/indigo carmine aluminum lake
100 mg tablets: yellow iron oxide
150 mg tablets: yellow iron oxide, red iron oxide, black iron oxide
200 mg tablets: FD&C Blue #2/indigo carmine aluminum lake
11.2 VIMPAT Injection
VIMPAT injection is a clear, colorless, sterile solution containing 10 mg lacosamide per mL for intravenous infusion. One 20-mL vial contains 200 mg of lacosamide drug substance. The inactive ingredients are sodium chloride and water for injection. Hydrochloric acid is used for pH adjustment. VIMPAT injection has a pH of 3.5 to 5.0.
11.3 VIMPAT Oral Solution
VIMPAT oral solution contains 10 mg of lacosamide per mL. The inactive ingredients are purified water, sorbitol solution, glycerin, polyethylene glycol, carboxymethylcellulose sodium, acesulfame potassium, methylparaben, flavoring (including natural and artificial flavors, propylene glycol, aspartame, and maltol), anhydrous citric acid and sodium chloride.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
The precise mechanism by which VIMPAT exerts its antiepileptic effects in humans remains to be fully elucidated. In vitro electrophysiological studies have shown that lacosamide selectively enhances slow inactivation of voltage-gated sodium channels, resulting in stabilization of hyperexcitable neuronal membranes and inhibition of repetitive neuronal firing.
12.2 Pharmacodynamics
A pharmacokinetic-pharmacodynamic (efficacy) analysis was performed based on the pooled data from the 3 efficacy trials for partial-onset seizures. Lacosamide exposure is correlated with the reduction in seizure frequency. However, doses above 400 mg/day do not appear to confer additional benefit in group analyses.
Cardiac Electrophysiology
Electrocardiographic effects of VIMPAT were determined in a double-blind, randomized clinical pharmacology trial of 247 healthy subjects. Chronic oral doses of 400 and 800 mg/day were compared with placebo and a positive control (400 mg moxifloxacin). VIMPAT did not prolong QTc interval and did not have a dose-related or clinically important effect on QRS duration. VIMPAT produced a small, dose-related increase in mean PR interval. At steady-state, the time of the maximum observed mean PR interval corresponded with tmax. The placebo-subtracted maximum increase in PR interval (at tmax) was 7.3 ms for the 400 mg/day group and 11.9 ms for the 800 mg/day group. For patients who participated in the controlled trials, the placebo-subtracted mean maximum increase in PR interval for a 400 mg/day VIMPAT dose was 3.1 ms in patients with partial-onset seizures and 9.4 ms for patients with diabetic neuropathy.
12.3 Pharmacokinetics
The pharmacokinetics of VIMPAT have been studied in healthy adult subjects (age range 18 to 87), adults with partial-onset seizures, adults with diabetic neuropathy, and subjects with renal and hepatic impairment.
VIMPAT is completely absorbed after oral administration with negligible first-pass effect with a high absolute bioavailability of approximately 100%. The maximum lacosamide plasma concentrations occur approximately 1 to 4 hour post-dose after oral dosing, and elimination half-life is approximately 13 hours. Steady state plasma concentrations are achieved after 3 days of twice daily repeated administration. Pharmacokinetics of VIMPAT are dose proportional (100-800 mg) and time invariant, with low inter- and intra-subject variability. Compared to lacosamide the major metabolite, O-desmethyl metabolite, has a longer Tmax (0.5 to 12 hours) and elimination half-life (15-23 hours).
Absorption and Bioavailability
VIMPAT is completely absorbed after oral administration. The oral bioavailability of VIMPAT tablets is approximately 100%. Food does not affect the rate and extent of absorption.
After intravenous administration, Cmax is reached at the end of infusion. The 30- and 60-minute intravenous infusions are bioequivalent to the oral tablet.
In a trial comparing the oral tablet with an oral solution containing 10 mg/mL lacosamide, bioequivalence between both formulations was shown.
Distribution
The volume of distribution is approximately 0.6 L/kg and thus close to the volume of total body water. VIMPAT is less than 15% bound to plasma proteins.
Metabolism and Elimination
VIMPAT is primarily eliminated from the systemic circulation by renal excretion and biotransformation.
After oral and intravenous administration of 100 mg [14C]-lacosamide approximately 95% of radioactivity administered was recovered in the urine and less than 0.5% in the feces. The major compounds excreted were unchanged lacosamide (approximately 40% of the dose), its O-desmethyl metabolite (approximately 30%), and a structurally unknown polar fraction (~20%). The plasma exposure of the major human metabolite, O-desmethyl-lacosamide, is approximately 10% of that of lacosamide. This metabolite has no known pharmacological activity.
The CYP isoforms mainly responsible for the formation of the major metabolite (O-desmethyl) are CYP3A4, CYP2C9, and CYP2C19. The elimination half-life of the unchanged drug is approximately 13 hours and is not altered by different doses, multiple dosing or intravenous administration.
There is no enantiomeric interconversion of lacosamide.
Special Populations
Renal impairment
Lacosamide and its major metabolite are eliminated from the systemic circulation primarily by renal excretion.
The AUC of VIMPAT was increased approximately 25% in mildly (CLCR 50-80 mL/min) and moderately (CLCR 30-50 mL/min) and 60% in severely (CLCR≤30mL/min) renally impaired patients compared to subjects with normal renal function (CLCR>80mL/min), whereas Cmax was unaffected. No dose adjustment is considered necessary in mildly and moderately renal impaired subjects. A maximum dose of 300 mg/day is recommended for patients with severe renal impairment (CLCR≤30mL/min) and in patients with endstage renal disease. VIMPAT is effectively removed from plasma by hemodialysis. Following a 4-hour hemodialysis treatment, AUC of VIMPAT is reduced by approximately 50%. Therefore dosage supplementation of up to 50% following hemodialysis should be considered. In all renally impaired patients, the dose titration should be performed with caution. [See Dosage and Administration (2.3) ]
Hepatic impairment
Lacosamide undergoes metabolism. Subjects with moderate hepatic impairment (Child-Pugh B) showed higher plasma concentrations of lacosamide (approximately 50-60% higher AUC compared to healthy subjects). The dose titration should be performed with caution in patients with hepatic impairment. A maximum dose of 300 mg/day is recommended for patients with mild or moderate hepatic impairment.
Patients with mild to moderate hepatic impairment should be observed closely during dose titration. A maximum dose of 300 mg/day is recommended for patients with mild to moderate hepatic impairment. The pharmacokinetics of lacosamide have not been evaluated in severe hepatic impairment. VIMPAT use is not recommended in patients with severe hepatic impairment. [See Dosage and Administration (2.3) ] Patients with co-existing hepatic and renal impairment should be monitored closely during dose titration.
Geriatric
In the elderly (>65 years), dose and body-weight normalized AUC and Cmax is about 20% increased compared to young subjects (18-64 years). This may be related to body weight and decreased renal function in elderly subjects. Dose reduction is not considered to be necessary.
Pediatric Patients
Pharmacokinetics of VIMPAT have not been studied in pediatric patients.
Gender
VIMPAT clinical trials indicate that gender does not have a clinically relevant influence on the pharmacokinetics of VIMPAT.
Race
There are no clinically relevant differences in the pharmacokinetics of VIMPAT between Asian, Black, and Caucasian subjects.
CYP2C19 Polymorphism
There are no clinically relevant differences in the pharmacokinetics of VIMPAT between CYP2C19 poor metabolizers and extensive metabolizers. Results from a trial in poor metabolizers (PM) (N=4) and extensive metabolizers (EM) (N=8) of cytochrome P450 (CYP) 2C19 showed that lacosamide plasma concentrations were similar in PMs and EMs, but plasma concentrations and the amount excreted into urine of the O-desmethyl metabolite were about 70% reduced in PMs compared to EMs.
Drug interactions
In Vitro Assessment of Drug Interactions
In vitro metabolism studies indicate that lacosamide does not induce the enzyme activity of drug metabolizing cytochrome P450 isoforms CYP1A2, 2B6, 2C9, 2C19 and 3A4. Lacosamide did not inhibit CYP 1A1, 1A2, 2A6, 2B6, 2C8, 2C9, 2D6, 2E1, 3A4/5 at plasma concentrations observed in clinical studies.
In vitro data suggest that lacosamide has the potential to inhibit CYP2C19 at therapeutic concentrations. However, an in vivo study with omeprazole did not show an inhibitory effect on omeprazole pharmacokinetics.
Lacosamide was not a substrate or inhibitor for P-glycoprotein.
Lacosamide is a substrate of CYP3A4, CYP2C9, and CYP2C19. Patients with renal or hepatic impairment who are taking strong inhibitors of CYP3A4 and CYP2C9 may have increased exposure to lacosamide.
Since <15% of lacosamide is bound to plasma proteins, a clinically relevant interaction with other drugs through competition for protein binding sites is unlikely.
In Vivo Assessment of Drug Interactions
Drug interaction studies with AEDs
Effect of VIMPAT on concomitant AEDs: VIMPAT 400 mg/day had no influence on the pharmacokinetics of 600 mg/day valproic acid and 400 mg/day carbamazepine in healthy subjects.
The placebo-controlled clinical studies in patients with partial-onset seizures showed that steady-state plasma concentrations of levetiracetam, carbamazepine, carbamazepine epoxide, lamotrigine, topiramate, oxcarbazepine monohydroxy derivative (MHD), phenytoin, valproic acid, phenobarbital, gabapentin, clonazepam, and zonisamide were not affected by concomitant intake of VIMPAT at any dose.
Effect of concomitant AEDs on VIMPAT: Drug-drug interaction studies in healthy subjects showed that 600 mg/day valproic acid had no influence on the pharmacokinetics of 400 mg/day VIMPAT. Likewise, 400 mg/day carbamazepine had no influence on the pharmacokinetics of VIMPAT in a healthy subject study. Population pharmacokinetics results in patients with partial-onset seizures showed small reductions (15% to 20% lower) in lacosamide plasma concentrations when VIMPAT was coadministered with carbamazepine, phenobarbital or phenytoin.
Drug-drug interaction studies with other drugs
Digoxin
There was no effect of VIMPAT (400 mg/day) on the pharmacokinetics of digoxin (0.5 mg once daily) in a study in healthy subjects.
Metformin
There were no clinically relevant changes in metformin levels following coadministration of VIMPAT (400 mg/day).
Metformin (500 mg three times a day) had no effect on the pharmacokinetics of VIMPAT (400 mg/day).
Omeprazole
Omeprazole is a CYP2C19 substrate and inhibitor.
There was no effect of VIMPAT (600 mg/day) on the pharmacokinetics of omeprazole (40 mg single dose) in healthy subjects. The data indicated that lacosamide had little in vivo inhibitory or inducing effect on CYP2C19.
Omeprazole at a dose of 40 mg once daily had no effect on the pharmacokinetics of VIMPAT (300 mg single dose). However, plasma levels of the O-desmethyl metabolite were reduced about 60% in the presence of omeprazole.
Midazolam
Midazolam is a 3A4 substrate.
There was no effect of VIMPAT (200 mg single dose or repeat doses of 400 mg/day given as 200 mg BID) on the pharmacokinetics of midazolam (single dose, 7.5 mg), indicating no inhibitory or inducing effects on CYP3A4.
Oral Contraceptives
There was no influence of VIMPAT (400 mg/day) on the pharmacodynamics and pharmacokinetics of an oral contraceptive containing 0.03 mg ethinylestradiol and 0.15 mg levonorgestrel in healthy subjects, except that a 20% increase in ethinylestradiol Cmax was observed.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
There was no evidence of drug related carcinogenicity in mice or rats. Mice and rats received lacosamide once daily by oral administration for 104 weeks at doses producing plasma exposures (AUC) up to approximately 1 and 3 times, respectively, the plasma AUC in humans at the maximum recommended human dose (MRHD) of 400 mg/day.
Lacosamide was negative in an in vitro Ames test and an in vivo mouse micronucleus assay. Lacosamide induced a positive response in the in vitro mouse lymphoma assay.
No adverse effects on male or female fertility or reproduction were observed in rats at doses producing plasma exposures (AUC) up to approximately 2 times the plasma AUC in humans at the MRHD.
14 CLINICAL STUDIES
14.1 Effectiveness in Partial-Onset Seizures
The efficacy of VIMPAT as adjunctive therapy in partial-onset seizures was established in three 12-week, randomized, double-blind, placebo-controlled, multicenter trials in adult patients. Patients enrolled had partial-onset seizures with or without secondary generalization and were not adequately controlled with 1 to 3 concomitant AEDs. During an 8-week baseline period, patients were required to have an average of ≥4 partial-onset seizures per 28 days with no seizure-free period exceeding 21 days. In these 3 trials, patients had a mean duration of epilepsy of 24 years and a median baseline seizure frequency ranging from 10 to 17 per 28 days. 84% of patients were taking 2 to 3 concomitant AEDs with or without concurrent vagal nerve stimulation.
Study 1 compared doses of VIMPAT 200, 400, and 600 mg/day with placebo. Study 2 compared doses of VIMPAT 400 and 600 mg/day with placebo. Study 3 compared doses of VIMPAT 200 and 400 mg/day with placebo. In all three trials, following an 8-week Baseline Phase to establish baseline seizure frequency prior to randomization, subjects were randomized and titrated to the randomized dose (a 1-step back-titration of VIMPAT 100 mg/day or placebo was allowed in the case of intolerable adverse events at the end of the Titration Phase). During the Titration Phase in all 3 trials, treatment was initiated at 100 mg/day (50 mg given twice daily) and increased in weekly increments of 100 mg/day to the target dose. The Titration Phase lasted 6 weeks in Study 1 and Study 2 and 4 weeks in Study 3. In all three trials, the Titration Phase was followed by a Maintenance Phase that lasted 12 weeks, during which patients were to remain on a stable dose of VIMPAT.
A reduction in 28 day seizure frequency (Baseline to Maintenance Phase) as compared to the placebo group was the primary variable in all three trials. The criteria for statistical significance was p<0.05. A statistically significant effect was observed with VIMPAT treatment (Figure 1) at doses of 200 mg/day (Study 3), 400 mg/day (Studies 1, 2, and 3), and 600 mg/day (Studies 1 and 2).
Subset evaluations of VIMPAT demonstrate no important differences in seizure control as a function of gender or race, although data on race was limited (about 10% of patients were non-Caucasian).
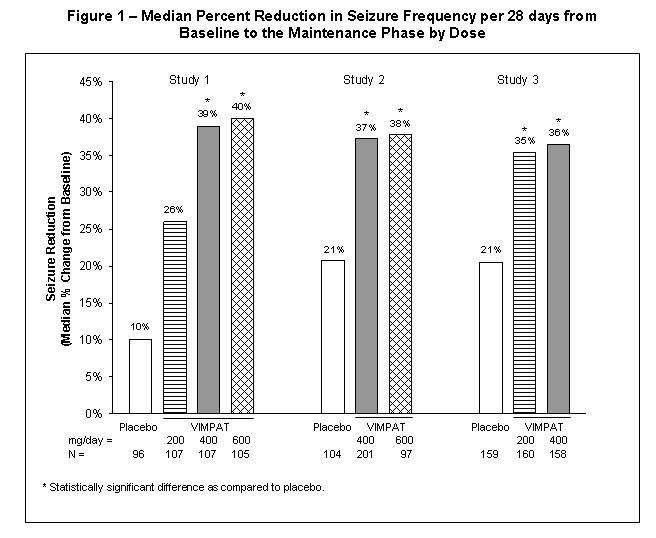
Figure 2 presents the percentage of patients (X-axis) with a percent reduction in partial seizure frequency (responder rate) from Baseline to the Maintenance phase at least as great as that represented on the Y-axis. A positive value on the Y-axis indicates an improvement from Baseline (i.e., a decrease in seizure frequency), while a negative value indicates a worsening from Baseline (i.e., an increase in seizure frequency). Thus, in a display of this type, a curve for an effective treatment is shifted to the left of the curve for placebo. The proportion of patients achieving any particular level of reduction in seizure frequency was consistently higher for the VIMPAT groups compared to the placebo group. For example, 40% of patients randomized to VIMPAT (400 mg/day) experienced a 50% or greater reduction in seizure frequency, compared to 23% of patients randomized to placebo. Patients with an increase in seizure frequency >100% are represented on the Y-axis as equal to or greater than -100%.

16 HOW SUPPLIED/STORAGE AND HANDLING
VIMPAT (lacosamide) Tablets 50 mg are pink, oval, film-coated tablets debossed with "SP" on one side and "50" on the other. They are supplied as follows:
| Bottles of 60 | NDC 0131-2477-35 |
| Unit Dose Carton of 60 tablets [6 cards, each card contains 10 tablets] | NDC 0131-2477-60 |
VIMPAT (lacosamide) Tablets 100 mg are dark yellow, oval, film-coated tablets debossed with "SP" on one side and "100" on the other. They are supplied as follows:
| Bottles of 60 | NDC 0131-2478-35 |
| Unit Dose Carton of 60 tablets [6 cards, each card contains 10 tablets] | NDC 0131-2478-60 |
VIMPAT (lacosamide) Tablets 150 mg are salmon, oval, film-coated tablets debossed with "SP" on one side and "150" on the other. They are supplied as follows:
| Bottles of 60 | NDC 0131-2479-35 |
| Unit Dose Carton of 60 tablets [6 cards, each card contains 10 tablets] | NDC 0131-2479-60 |
VIMPAT (lacosamide) Tablets 200 mg are blue, oval, film-coated tablets debossed with "SP" on one side and "200" on the other. They are supplied as follows:
| Bottles of 60 | NDC 0131-2480-35 |
| Unit Dose Carton of 60 tablets [6 cards, each card contains 10 tablets] | NDC 0131-2480-60 |
VIMPAT (lacosamide) injection 200 mg/20 mL is a clear, colorless sterile solution supplied in 20 mL colorless single-use glass vials.
| 200 mg/20 mL vial in cartons of 10 vials | NDC 0131-1810-67 |
VIMPAT (lacosamide) oral solution 10 mg/mL is a clear, colorless to yellow or yellow-brown, strawberry-flavored liquid. It is supplied in PET bottles as follows:
| 200 mL bottles | NDC 0131-5410-71 |
| 465 mL bottles | NDC 0131-5410-70 |
16.1 Storage
Store at 20°C to 25°C (68°F to 77°F); excursions permitted between 15°C to 30°C (59°F to 86°F). [See USP Controlled Room Temperature]
Do not freeze VIMPAT injection or oral solution. Discard any unused VIMPAT oral solution remaining after seven (7) weeks of first opening the bottle.
17 PATIENT COUNSELING INFORMATION
[See Medication Guide]
Patients should be informed of the availability of a Medication Guide, and they should be instructed to read the Medication Guide prior to taking VIMPAT. Patients should be instructed to take VIMPAT only as prescribed.
17.1 Suicidal Thinking and Behavior
Patients, their caregivers, and families should be counseled that AEDs, including VIMPAT, may increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
17.2 Dizziness and Ataxia
Patients should be counseled that VIMPAT use may cause dizziness, double vision, abnormal coordination and balance, and somnolence. Patients taking VIMPAT should be advised not to drive, operate complex machinery, or engage in other hazardous activities until they have become accustomed to any such effects associated with VIMPAT.
17.3 Cardiac Rhythm and Conduction Abnormalities
Patients should be counseled that VIMPAT is associated with electrocardiographic changes that may predispose to irregular beat and syncope, particularly in patients with underlying cardiovascular disease, with heart conduction problems or who are taking other medications that affect the heart. Patients who develop syncope should lay down with raised legs and contact their health care provider.
17.4 Multiorgan Hypersensitivity Reactions
Patients should be aware that VIMPAT may cause serious hypersensitivity reactions affecting multiple organs such as the liver and kidney. VIMPAT should be discontinued if a serious hypersensitivity reaction is suspected. Patients should also be instructed to report promptly to their physicians any symptoms of liver toxicity (e.g. fatigue, jaundice, dark urine).
17.5 Pregnancy Registry
UCB, Inc. has established the UCB AED Pregnancy Registry to advance scientific knowledge about safety and outcomes in pregnant women being treated with VIMPAT. To ensure broad program access and reach, either a healthcare provider or the patient can initiate enrollment in the UCB AED Pregnancy Registry by calling 1-888-537-7734 (toll free).
Patients should also be encouraged to enroll in the North American Antiepileptic Drug Pregnancy Registry if they become pregnant. This Registry is collecting information about the safety of AEDs during pregnancy. To enroll, patients can call the toll free number 1-888-233-2334. [See Use in Specific Populations (8.1) ]
Medication Guide
VIMPAT (VIM-păt) CV
(lacosamide)
Tablet, Oral Solution and Injection for Intravenous Use
Read this Medication Guide before you start taking VIMPAT and each time you get a refill. There may be new information. This Medication Guide describes important safety information about VIMPAT. This information does not take the place of talking to your healthcare provider about your medical condition or treatment.
What is the most important information I should know about VIMPAT?
Do not stop taking VIMPAT without first talking to your healthcare provider.
Stopping VIMPAT suddenly can cause serious problems.
VIMPAT can cause serious side effects, including:
-
1. Like other antiepileptic drugs, VIMPAT may cause suicidal thoughts or actions in a very small number of people, about 1 in 500.
Call a healthcare provider right away if you have any of these symptoms, especially if they are new, worse, or worry you:- thoughts about suicide or dying
- attempt to commit suicide
- new or worse depression
- new or worse anxiety
- feeling agitated or restless
- panic attacks
- trouble sleeping (insomnia)
- new or worse irritability
- acting aggressive, being angry, or violent
- acting on dangerous impulses
- an extreme increase in activity and talking (mania)
- other unusual changes in behavior or mood
How can I watch for early symptoms of suicidal thoughts and actions?- Pay attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings.
- Keep all follow-up visits with your healthcare provider as scheduled.
- Call your healthcare provider between visits as needed, especially if you are worried about symptoms.
- Suicidal thoughts or actions can be caused by things other than medicines. If you have suicidal thoughts or actions, your healthcare provider may check for other causes.
- Do not stop VIMPAT without first talking to a healthcare provider. Stopping VIMPAT suddenly can cause serious problems. Stopping seizure medicine suddenly in a patient who has epilepsy can cause seizures that will not stop (status epilepticus).
-
2. VIMPAT may cause you to feel dizzy, have double vision, feel sleepy, or have problems with coordination and walking. Do not drive, operate heavy machinery, or do other dangerous activities until you know how VIMPAT affects you. -
3. VIMPAT may cause you to have an irregular heartbeat or may cause you to faint. Call your healthcare provider if you have:- fast, slow, or pounding heartbeat
- shortness of breath
- feel lightheaded
- fainted or if you feel like you are going to faint
If you have fainted or feel like you are going to faint you should lay down with your legs raised. -
4. VIMPAT is a federally controlled substance (C-V) because it can be abused or lead to drug dependence. Keep your VIMPAT in a safe place, to protect it from theft. Never give your VIMPAT to anyone else, because it may harm them. Selling or giving away this medicine is against the law.
What is VIMPAT?
VIMPAT is a prescription medicine used with other medicines to treat partial-onset seizures in people 17 years of age and older.
What should I tell my healthcare provider before taking VIMPAT?
Before you take VIMPAT, tell your healthcare provider, if you:
- have or have had depression, mood problems or suicidal thoughts or behavior
- have heart problems
- have kidney problems
- have liver problems
- have abused prescription medicines, street drugs or alcohol in the past
- have any other medical problems
- are pregnant or plan to become pregnant. It is not known if VIMPAT can harm your unborn baby. Tell your healthcare provider right away if you become pregnant while taking VIMPAT. You and your healthcare provider will decide if you should take VIMPAT while you are pregnant.
- If you become pregnant while taking VIMPAT, talk to your healthcare provider about registering with the North American Antiepileptic Drug Pregnancy Registry. You can enroll in this registry by calling 1-888-233-2334. You can also enroll in the UCB AED Pregnancy Registry by calling 1-888-537-7734. The purpose of this registry is to collect information about the safety of antiepileptic medicine during pregnancy.
- are breastfeeding or plan to breastfeed. It is not known if VIMPAT passes into your breast milk or if it can harm your baby. Talk to your healthcare provider about the best way to feed your baby if you take VIMPAT.
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements.
Taking VIMPAT with certain other medicines may cause side effects or affect how well they work. Do not start or stop other medicines without talking to your healthcare provider. Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist each time you get a new medicine.
How should I take VIMPAT?
- Take VIMPAT exactly as your healthcare provider tells you.
- Your healthcare provider will tell you how much VIMPAT to take and when to take it.
- Your healthcare provider may change your dose if needed.
- Do not stop VIMPAT without first talking to a healthcare provider. Stopping VIMPAT suddenly in a patient who has epilepsy can cause seizures that will not stop (status epilepticus).
- VIMPAT may be taken with or without food.
- If your healthcare provider has prescribed VIMPAT oral solution, be sure to ask your pharmacist for a medicine dropper or medicine cup to help you measure the correct amount of VIMPAT oral solution. Do not use a household teaspoon. Ask your pharmacist for instructions on how to use the measuring device the right way.
- If you take too much VIMPAT, call your healthcare provider or local Poison Control Center right away.
What should I avoid while taking VIMPAT?
-
What are the possible side effects of VIMPAT?
See "What is the most important information I should know about VIMPAT?".
VIMPAT may cause other serious side effects including:
VIMPAT may cause a serious allergic reaction that may affect your skin or other parts of your body such as your liver or blood cells. Call your healthcare provider right away if you have:
- a skin rash, hives
- fever or swollen glands that do not go away
- shortness of breath, swelling of the legs, yellowing of the skin or whites of the eyes, or dark urine.
The most common side effects of VIMPAT include:
- dizziness
- headache
- double vision
- nausea
These are not all of the possible side effects of VIMPAT. For more information ask your healthcare provider or pharmacist. Tell your healthcare provider about any side effect that bothers you or that does not go away. Call your healthcare provider for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store VIMPAT?
- Store VIMPAT between 59°F to 86°F (15°C to 30°C)
Keep VIMPAT and all medicines out of the reach of children
General Information about VIMPAT
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use VIMPAT for a condition for which it was not prescribed. Do not give VIMPAT to other people, even if they have the same symptoms that you have. It may harm them.
This Medication Guide summarizes the most important information about VIMPAT. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about VIMPAT that is written for health professionals.
For more information, go to www.vimpat.com or call 1-800-477-7877.
What are the ingredients in VIMPAT?
-
-
- 50 mg tablets: red iron oxide, black iron oxide, FD&C Blue #2/indigo carmine aluminum lake
- 100 mg tablets: yellow iron oxide
- 150 mg tablets: yellow iron oxide, red iron oxide, black iron oxide
- 200 mg tablets: FD&C Blue #2/indigo carmine aluminum lake
-
-
Manufactured for
UCB, Inc.
Smyrna, GA 30080
Issued 09/2013
This Medication Guide has been approved by the U.S. Food and Drug Administration.
VIMPAT® is a registered trademark under license from Harris FRC Corporation and covered by one or more claims of U.S. Patent 38,551.
PRINCIPAL DISPLAY PANEL - 50 mg Bottle Label
NDC 0131-2477-35
VIMPAT®
(lacosamide) tablets CV
50 mg
Rx only
60 tablets
ATTENTION PHARMACIST:
Each patient is required to receive the
accompanying Medication Guide.

PRINCIPAL DISPLAY PANEL - 100 mg Bottle Label
NDC 0131-2478-35
VIMPAT®
(lacosamide) tablets CV
100 mg
Rx only
60 tablets
ATTENTION PHARMACIST:
Each patient is required to receive the
accompanying Medication Guide.

PRINCIPAL DISPLAY PANEL - 150 mg Bottle Label
NDC 0131-2479-35
VIMPAT®
(lacosamide) tablets CV
150 mg
Rx only
60 tablets
ATTENTION PHARMACIST:
Each patient is required to receive the
accompanying Medication Guide.

PRINCIPAL DISPLAY PANEL - 200 mg Bottle Label
NDC 0131-2480-35
VIMPAT®
(lacosamide) tablets CV
200 mg
Rx only
60 tablets
ATTENTION PHARMACIST:
Each patient is required to receive the
accompanying Medication Guide.
PRINCIPAL DISPLAY PANEL - Kit Carton
2 Week
Starter Kit
VIMPAT
®
(lacosamide) tablets CV
ATTENTION PHYSICIAN:
Each patient is required to receive
the accompanying Medication Guide.
Not for Sale
Professional Samples

PRINCIPAL DISPLAY PANEL - 200 mg/20 mL Vial Carton
NDC 0131-1810-67
Rx Only
Intravenous Use Only
10 vials
VIMPAT
®
(lacosamide) injection CV
200 mg /20 mL
(10 mg/mL)
Manufactured for:
UCB, Inc.
Smyrna, GA 30080

PRINCIPAL DISPLAY PANEL - 465 mL Bottle Label
NDC 0131-5410-70
VIMPAT
®
(lacosamide) oral solution CV
10 mg / mL
Rx only
ATTENTION PHARMACIST:
Each patient is required to receive the
accompanying Medication Guide.
Manufactured for:
UCB, Inc.
Smyrna, GA 30080
465 mL

Vimpatlacosamide TABLET, FILM COATED
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Vimpatlacosamide TABLET, FILM COATED
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Vimpatlacosamide TABLET, FILM COATED
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Vimpatlacosamide TABLET, FILM COATED
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Vimpatlacosamide KIT
| |||||||||||||||||||||||||||||||||||||||||||||
Vimpatlacosamide INJECTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Vimpatlacosamide SOLUTION
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||