Xopenex
Xopenex® (levalbuterol HCl) Inhalation Solution 0.31 mg*, 0.63 mg*, 1.25 mg*
FULL PRESCRIBING INFORMATION: CONTENTS*
- SPL UNCLASSIFIED
- XOPENEX DESCRIPTION
- CLINICAL PHARMACOLOGY
- INDICATIONS & USAGE
- XOPENEX CONTRAINDICATIONS
- WARNINGS
- PRECAUTIONS
- XOPENEX ADVERSE REACTIONS
- XOPENEX ADVERSE REACTIONS
- SPL UNCLASSIFIED
- OVERDOSAGE
- DOSAGE & ADMINISTRATION
- HOW SUPPLIED
- SPL PATIENT PACKAGE INSERT
- PACKAGE LABEL.PRINCIPAL DISPLAY PANEL SECTION
FULL PRESCRIBING INFORMATION
SPL UNCLASSIFIED
*Potency expressed as levalbuterol
PRESCRIBING INFORMATION
XOPENEX DESCRIPTION
Xopenex (levalbuterol HCl) Inhalation Solution is a sterile, clear, colorless, preservative-free solution of the hydrochloride salt of levalbuterol, the (R)-enantiomer of the drug substance racemic albuterol. Levalbuterol HCl is a relatively selective beta2-adrenergic receptor agonist (see CLINICAL PHARMACOLOGY ). The chemical name for levalbuterol HCl is (R)-α1-[[(1,1-dimethylethyl)amino]methyl]-4-hydroxy-1,3-benzenedimethanol hydrochloride, and its established chemical structure is as follows:
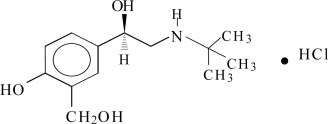
The molecular weight of levalbuterol HCl is 275.8, and its empirical formula is C13H21NO3•HCl. It is a white to off-white, crystalline solid, with a melting point of approximately 187°C and solubility of approximately 180 mg/mL in water.
Levalbuterol HCl is the USAN modified name for (R)-albuterol HCl in the United States.
Xopenex (levalbuterol HCl) Inhalation Solution is supplied in unit-dose vials and requires no dilution before administration by nebulization. Each 3 mL unit-dose vial contains 0.31 mg of levalbuterol (as 0.36 mg of levalbuterol HCl) or 0.63 mg of levalbuterol (as 0.73 mg of levalbuterol HCl) or 1.25 mg of levalbuterol (as 1.44 mg of levalbuterol HCl), sodium chloride to adjust tonicity, and sulfuric acid to adjust the pH to 4.0 (3.3 to 4.5).
CLINICAL PHARMACOLOGY
Activation of beta2-adrenergic receptors on airway smooth muscle leads to the activation of adenylcyclase and to an increase in the intracellular concentration of cyclic-3´, 5´-adenosine monophosphate (cyclic AMP). This increase in cyclic AMP leads to the activation of protein kinase A, which inhibits the phosphorylation of myosin and lowers intracellular ionic calcium concentrations, resulting in relaxation. Levalbuterol relaxes the smooth muscles of all airways, from the trachea to the terminal bronchioles. Levalbuterol acts as a functional antagonist to relax the airway irrespective of the spasmogen involved, thus protecting against all bronchoconstrictor challenges. Increased cyclic AMP concentrations are also associated with the inhibition of release of mediators from mast cells in the airway.
While it is recognized that beta2-adrenergic receptors are the predominant receptors on bronchial smooth muscle, data indicate that there is a population of beta2-receptors in the human heart that comprise between 10% and 50% of cardiac beta-adrenergic receptors. The precise function of these receptors has not been established (see WARNINGS ). However, all beta-adrenergic agonist drugs can produce a significant cardiovascular effect in some patients, as measured by pulse rate, blood pressure, symptoms, and/or electrocardiographic changes.
Results from an in vitro study of binding to human beta-adrenergic receptors demonstrated that levalbuterol has approximately 2-fold greater binding affinity than racemic albuterol and approximately 100-fold greater binding affinity than (S)-albuterol. In guinea pig airways, levalbuterol HCl and racemic albuterol decreased the response to spasmogens (e.g., acetylcholine and histamine), whereas (S)-albuterol was ineffective. These results suggest that the bronchodilatory effects of racemic albuterol are attributable to the (R)-enantiomer.
Intravenous studies in rats with racemic albuterol sulfate have demonstrated that albuterol crosses the blood-brain barrier and reaches brain concentrations amounting to approximately 5.0% of the plasma concentrations. In structures outside the blood-brain barrier (pineal and pituitary glands), albuterol concentrations were found to be 100 times those in the whole brain.
Studies in laboratory animals (minipigs, rodents, and dogs) have demonstrated the occurrence of cardiac arrhythmias and sudden death (with histologic evidence of myocardial necrosis) when beta-agonists and methylxanthines are administered concurrently. The clinical significance of these findings is unknown.
The inhalation pharmacokinetics of Xopenex Inhalation Solution were investigated in a randomized cross-over study in 30 healthy adults following administration of a single dose of 1.25 mg and a cumulative dose of 5 mg of Xopenex Inhalation Solution and a single dose of 2.5 mg and a cumulative dose of 10 mg of racemic albuterol sulfate inhalation solution by nebulization using a PARI LC Jet™ nebulizer with a Dura-Neb® 2000 compressor.
Following administration of a single 1.25 mg dose of Xopenex Inhalation Solution, exposure to (R)-albuterol (AUC of 3.3 ng•hr/mL) was approximately 2-fold higher than following administration of a single 2.5 mg dose of racemic albuterol inhalation solution (AUC of 1.7 ng•hr/mL) (see Table 1 ). Following administration of a cumulative 5 mg dose of Xopenex Inhalation Solution (1.25 mg given every 30 minutes for a total of four doses) or a cumulative 10 mg dose of racemic albuterol inhalation solution (2.5 mg given every 30 minutes for a total of four doses), Cmax and AUC of (R)-albuterol were comparable (see Table 1 ).
| Single Dose | Cumulative Dose | |||||
| Xopenex 1.25 mg | Racemic albuterol sulfate 2.5 mg |
Xopenex 5 mg | Racemic albuterol sulfate 10 mg |
|||
| Cmax (ng/mL) | ||||||
| (R)-albuterol | 1.1 (0.45) | 0.8 (0.41)** | 4.5 (2.20) | 4.2 (1.51)** | ||
| Tmax (h)γ | ||||||
| (R)-albuterol | 0.2 (0.17, 0.37) | 0.2 (0.17, 1.50) | 0.2 (–0.18*, 1.25) | 0.2 (–0.28*, 1.00) | ||
| AUC (ng•h/mL) | ||||||
| (R)-albuterol | 3.3 (1.58) | 1.7 (0.99)** | 17.4 (8.56) | 16.0 (7.12)** | ||
| T½ (h) | ||||||
| (R)-albuterol | 3.3 (2.48) | 1.5 (0.61) | 4.0 (1.05) | 4.1 (0.97) | ||
|
γ Median (Min, Max) reported for Tmax. |
||||||
|
* A negative Tmax indicates Cmax occurred between first and last nebulizations. |
||||||
|
** Values reflect only (R)-albuterol and do not include (S)-albuterol. |
The pharmacokinetic parameters of (R)- and (S)-albuterol in children with asthma were obtained using population pharmacokinetic analysis. These data are presented in Table 2 . For comparison, adult data obtained by conventional pharmacokinetic analysis from a different study also are presented in Table 2 .
In children, AUC and Cmax of (R)-albuterol following administration of 0.63 mg Xopenex Inhalation Solution were comparable to those following administration of 1.25 mg racemic albuterol sulfate inhalation solution.
When the same dose of 0.63 mg of Xopenex was given to children and adults, the predicted Cmax of (R)–albuterol in children was similar to that in adults (0.52 vs. 0.56 ng/mL), while predicted AUC in children (2.55 ng•hr/mL) was about 1.5-fold higher than that in adults (1.65 ng•hr/mL). These data support lower doses for children 6-11 years old compared with the adult doses (see DOSAGE AND ADMINISTRATION ).
| Children 6-11 years | Adults ≥12 years | ||||||
| Treatment | Xopenex 0.31 mg |
Xopenex 0.63 mg |
Racemic albuterol 1.25mg |
Racemic albuterol 2.5 mg |
Xopenex 0.63 mg |
Xopenex 1.25 mg |
|
| AUC0-∞ (ng•hr/mL) c | 1.36 | 2.55 | 2.65 | 5.02 | 1.65 a | 3.3 b | |
| Cmax (ng/mL) d | 0.303 | 0.521 | 0.553 | 1.08 | 0.56 a | 1.1 b | |
|
a The values are predicted by assuming linear pharmacokinetics |
|||||||
|
b The data obtained from Table 1 |
|||||||
|
c Area under the plasma concentration curve from time 0 to infinity |
|||||||
|
d Maximum plasma concentration |
Information available in the published literature suggests that the primary enzyme responsible for the metabolism of albuterol enantiomers in humans is SULT1A3 (sulfotransferase). When racemic albuterol was administered either intravenously or via inhalation after oral charcoal administration, there was a 3- to 4-fold difference in the area under the concentration-time curves between the (R)- and (S)-albuterol enantiomers, with (S)-albuterol concentrations being consistently higher. However, without charcoal pretreatment, after either oral or inhalation administration the differences were 8- to 24-fold, suggesting that (R)-albuterol is preferentially metabolized in the gastrointestinal tract, presumably by SULT1A3.
The primary route of elimination of albuterol enantiomers is through renal excretion (80% to 100%) of either the parent compound or the primary metabolite. Less than 20% of the drug is detected in the feces. Following intravenous administration of racemic albuterol, between 25% and 46% of the (R)-albuterol fraction of the dose was excreted as unchanged (R)-albuterol in the urine.
Hepatic Impairment: The effect of hepatic impairment on the pharmacokinetics of Xopenex Inhalation Solution has not been evaluated.
Renal Impairment: The effect of renal impairment on the pharmacokinetics of racemic albuterol was evaluated in 5 subjects with creatinine clearance of 7 to 53 mL/min, and the results were compared with those from healthy volunteers. Renal disease had no effect on the half-life, but there was a 67% decline in racemic albuterol clearance. Caution should be used when administering high doses of Xopenex Inhalation Solution to patients with renal impairment.
In a randomized, double-blind, placebo-controlled, cross-over study, 20 adults with mild-to-moderate asthma received single doses of Xopenex Inhalation Solution (0.31, 0.63, and 1.25 mg) and racemic albuterol sulfate inhalation solution (2.5 mg). All doses of active treatment produced a significantly greater degree of bronchodilation (as measured by percent change from pre-dose mean FEV1) than placebo, and there were no significant differences between any of the active treatment arms. The bronchodilator responses to 1.25 mg of Xopenex Inhalation Solution and 2.5 mg of racemic albuterol sulfate inhalation solution were clinically comparable over the 6-hour evaluation period, except for a slightly longer duration of action (>15% increase in FEV1 from baseline) after administration of 1.25 mg of Xopenex Inhalation Solution. Systemic beta-adrenergic adverse effects were observed with all active doses and were generally dose-related for (R)-albuterol. Xopenex Inhalation Solution at a dose of 1.25 mg produced a slightly higher rate of systemic beta-adrenergic adverse effects than the 2.5 mg dose of racemic albuterol sulfate inhalation solution.
In a randomized, double-blind, placebo-controlled, cross-over study, 12 adults with mild-to-moderate asthma were challenged with inhaled methacholine chloride 20 and 180 minutes following administration of a single dose of 2.5 mg of racemic albuterol sulfate, 1.25 mg of Xopenex, 1.25 mg of (S)-albuterol, or placebo using a PARI LC Jet™ nebulizer. Racemic albuterol sulfate, Xopenex, and (S)-albuterol had a protective effect against methacholine-induced bronchoconstriction 20 minutes after administration, although the effect of (S)-albuterol was minimal. At 180 minutes after administration, the bronchoprotective effect of 1.25 mg of Xopenex was comparable to that of 2.5 mg of racemic albuterol sulfate. At 180 minutes after administration, 1.25 mg of (S)-albuterol had no bronchoprotective effect.
In a clinical study in adults with mild-to-moderate asthma, comparable efficacy (as measured by change from baseline FEV1) and safety (as measured by heart rate, blood pressure, ECG, serum potassium, and tremor) were demonstrated after a cumulative dose of 5 mg of Xopenex Inhalation Solution (four consecutive doses of 1.25 mg administered every 30 minutes) and 10 mg of racemic albuterol sulfate inhalation solution (four consecutive doses of 2.5 mg administered every 30 minutes).
The safety and efficacy of Xopenex Inhalation Solution were evaluated in a 4-week, multicenter, randomized, double-blind, placebo-controlled, parallel-group study in 362 adult and adolescent patients 12 years of age and older, with mild-to-moderate asthma (mean baseline FEV1 60% of predicted). Approximately half of the patients were also receiving inhaled corticosteroids. Patients were randomized to receive Xopenex 0.63 mg, Xopenex 1.25 mg, racemic albuterol sulfate 1.25 mg, racemic albuterol sulfate 2.5 mg, or placebo three times a day administered via a PARI LC Plus™ nebulizer and a Dura-Neb® portable compressor. Racemic albuterol delivered by a chlorofluorocarbon (CFC) metered dose inhaler (MDI) was used on an as-needed basis as the rescue medication.
Efficacy, as measured by the mean percent change from baseline FEV1, was demonstrated for all active treatment regimens compared with placebo on day 1 and day 29. On both day 1 (see
Figure 1
) and day 29 (see
Figure 2
), 1.25 mg of Xopenex demonstrated the largest mean percent change from baseline FEV1 compared with the other active treatments. A dose of 0.63 mg of Xopenex and 2.5 mg of racemic albuterol sulfate produced a clinically comparable mean percent change from baseline FEV1 on both day 1 and day 29.
Figure 1: Mean Percent Change from Baseline FEV1 on Day 1, Adults and Adolescents ≥12 years old

Figure 2: Mean Percent Change from Baseline FEV1 on Day 29, Adults and Adolescents ≥12 years old
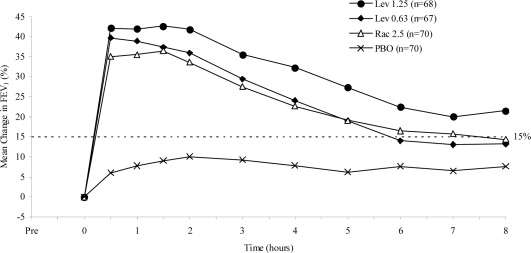
The mean time to onset of a 15% increase in FEV1 over baseline for levalbuterol at doses of 0.63 mg and 1.25 mg was approximately 17 minutes and 10 minutes, respectively, and the mean time to peak effect for both doses was approximately 1.5 hours after 4 weeks of treatment. The mean duration of effect, as measured by a >15% increase from baseline FEV1, was approximately 5 hours after administration of 0.63 mg of levalbuterol and approximately 6 hours after administration of 1.25 mg of levalbuterol after 4 weeks of treatment. In some patients, the duration of effect was as long as 8 hours.
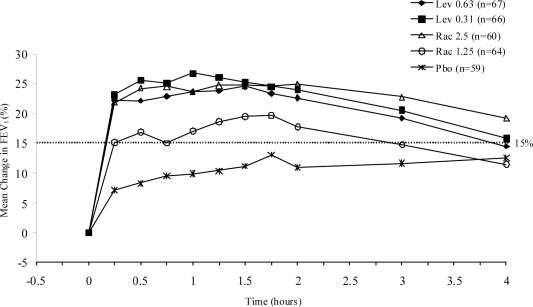
A multi-center, randomized, double-blind, placebo- and active-controlled study was conducted in children with mild-to-moderate asthma (mean baseline FEV1 73% of predicted) (n=316). Following a 1-week placebo run-in, subjects were randomized to Xopenex (0.31 or 0.63 mg), racemic albuterol (1.25 or 2.5 mg), or placebo, which were delivered three times a day for 3 weeks using a PARI LC Plus™ nebulizer and a Dura-Neb® 3000 compressor.
Efficacy, as measured by mean peak percent change from baseline FEV1, was demonstrated for all active treatment regimens compared with placebo on day 1 and day 21. Time profile FEV1 curves for day 1 and day 21 are shown in
Figure 3
and
Figure 4
, respectively. The onset of effect (time to a 15% increase in FEV1 over test-day baseline) and duration of effect (maintenance of a >15% increase in FEV1 over test-day baseline) of levalbuterol were clinically comparable to those of racemic albuterol.
Figure 3: Mean Percent Change from Baseline FEV1 on Day 1, Children 6-11 Years of Age

Figure 4: Mean Percent Change from Baseline FEV1 on Day 21, Children 6-11 Years of Age
INDICATIONS & USAGE
Xopenex (levalbuterol HCl) Inhalation Solution is indicated for the treatment or prevention of bronchospasm in adults, adolescents, and children 6 years of age and older with reversible obstructive airway disease.
XOPENEX CONTRAINDICATIONS
Xopenex (levalbuterol HCl) Inhalation Solution is contraindicated in patients with a history of hypersensitivity to levalbuterol HCl or racemic albuterol.
WARNINGS
- Paradoxical Bronchospasm: Like other inhaled beta-adrenergic agonists, Xopenex Inhalation Solution can produce paradoxical bronchospasm, which may be life threatening. If paradoxical bronchospasm occurs, Xopenex Inhalation Solution should be discontinued immediately and alternative therapy instituted. It should be recognized that paradoxical bronchospasm, when associated with inhaled formulations, frequently occurs with the first use of a new canister or vial.
- Deterioration of Asthma: Asthma may deteriorate acutely over a period of hours or chronically over several days or longer. If the patient needs more doses of Xopenex Inhalation Solution than usual, this may be a marker of destabilization of asthma and requires reevaluation of the patient and treatment regimen, giving special consideration to the possible need for anti-inflammatory treatment, e.g., corticosteroids.
- Use of Anti-Inflammatory Agents: The use of beta-adrenergic agonist bronchodilators alone may not be adequate to control asthma in many patients. Early consideration should be given to adding anti-inflammatory agents, e.g., corticosteroids, to the therapeutic regimen.
- Cardiovascular Effects: Xopenex Inhalation Solution, like all other beta-adrenergic agonists, can produce a clinically significant cardiovascular effect in some patients, as measured by pulse rate, blood pressure, and/or symptoms. Although such effects are uncommon after administration of Xopenex Inhalation Solution at recommended doses, if they occur, the drug may need to be discontinued. In addition, beta-agonists have been reported to produce ECG changes, such as flattening of the T wave, prolongation of the QTc interval, and ST segment depression. The clinical significance of these findings is unknown. Therefore, Xopenex Inhalation Solution, like all sympathomimetic amines, should be used with caution in patients with cardiovascular disorders, especially coronary insufficiency, cardiac arrhythmias, and hypertension.
- Do Not Exceed Recommended Dose: Fatalities have been reported in association with excessive use of inhaled sympathomimetic drugs in patients with asthma. The exact cause of death is unknown, but cardiac arrest following an unexpected development of a severe acute asthmatic crisis and subsequent hypoxia is suspected.
- Immediate Hypersensitivity Reactions: Immediate hypersensitivity reactions may occur after administration of racemic albuterol, as demonstrated by rare cases of urticaria, angioedema, rash, bronchospasm, anaphylaxis, and oropharyngeal edema. The potential for hypersensitivity must be considered in the clinical evaluation of patients who experience immediate hypersensitivity reactions while receiving Xopenex Inhalation Solution.
PRECAUTIONS
Levalbuterol HCl, like all sympathomimetic amines, should be used with caution in patients with cardiovascular disorders, especially coronary insufficiency, hypertension, and cardiac arrhythmias; in patients with convulsive disorders, hyperthyroidism, or diabetes mellitus; and in patients who are unusually responsive to sympathomimetic amines. Clinically significant changes in systolic and diastolic blood pressure have been seen in individual patients and could be expected to occur in some patients after the use of any beta-adrenergic bronchodilator.
Large doses of intravenous racemic albuterol have been reported to aggravate preexisting diabetes mellitus and ketoacidosis. As with other beta-adrenergic agonist medications, levalbuterol may produce significant hypokalemia in some patients, possibly through intracellular shunting, which has the potential to produce adverse cardiovascular effects. The decrease is usually transient, not requiring supplementation.
See illustrated Patient's Instructions for Use.
The action of Xopenex (levalbuterol HCl) Inhalation Solution may last up to 8 hours. Xopenex Inhalation Solution should not be used more frequently than recommended. Do not increase the dose or frequency of dosing of Xopenex Inhalation Solution without consulting your physician. If you find that treatment with Xopenex Inhalation Solution becomes less effective for symptomatic relief, your symptoms become worse, and/or you need to use the product more frequently than usual, you should seek medical attention immediately. While you are taking Xopenex Inhalation Solution, other inhaled drugs and asthma medications should be taken only as directed by your physician. Common adverse effects include palpitations, chest pain, rapid heart rate, headache, dizziness, and tremor or nervousness. If you are pregnant or nursing, contact your physician about the use of Xopenex Inhalation Solution.
Effective and safe use of Xopenex Inhalation Solution requires consideration of the following information in addition to that provided under Patient's Instructions for Use:
Xopenex Inhalation Solution single-use low-density polyethylene (LDPE) vials should be protected from light and excessive heat. Store in the protective foil pouch between 20°C and 25°C (68°F and 77°F) [see USP Controlled Room Temperature]. Do not use after the expiration date stamped on the container. Unused vials should be stored in the protective foil pouch. Once the foil pouch is opened, the vials should be used within 2 weeks. Vials removed from the pouch, if not used immediately, should be protected from light and used within 1 week. Discard any vial if the solution is not colorless.
The drug compatibility (physical and chemical), efficacy, and safety of Xopenex Inhalation Solution when mixed with other drugs in a nebulizer have not been established.
Other short-acting sympathomimetic aerosol bronchodilators or epinephrine should be used with caution with levalbuterol. If additional adrenergic drugs are to be administered by any route, they should be used with caution to avoid deleterious cardiovascular effects.
- Beta-blockers: Beta-adrenergic receptor blocking agents not only block the pulmonary effect of beta-agonists such as Xopenex (levalbuterol HCl) Inhalation Solution, but may also produce severe bronchospasm in asthmatic patients. Therefore, patients with asthma should not normally be treated with beta-blockers. However, under certain circumstances, e.g., prophylaxis after myocardial infarction, there may be no acceptable alternatives to the use of beta-adrenergic blocking agents in patients with asthma. In this setting, cardioselective beta-blockers could be considered, although they should be administered with caution.
- Diuretics: The ECG changes and/or hypokalemia that may result from the administration of non-potassium sparing diuretics (such as loop or thiazide diuretics) can be acutely worsened by beta-agonists, especially when the recommended dose of the beta-agonist is exceeded. Although the clinical significance of these effects is not known, caution is advised in the coadministration of beta-agonists with non-potassium sparing diuretics.
- Digoxin: Mean decreases of 16% and 22% in serum digoxin levels were demonstrated after single-dose intravenous and oral administration of racemic albuterol, respectively, to normal volunteers who had received digoxin for 10 days. The clinical significance of these findings for patients with obstructive airway disease who are receiving levalbuterol HCl and digoxin on a chronic basis is unclear. Nevertheless, it would be prudent to carefully evaluate the serum digoxin levels in patients who are currently receiving digoxin and Xopenex Inhalation Solution.
- Monoamine Oxidase Inhibitors or Tricyclic Antidepressants: Xopenex Inhalation Solution should be administered with extreme caution to patients being treated with monoamine oxidase inhibitors or tricyclic antidepressants, or within 2 weeks of discontinuation of such agents, because the action of levalbuterol HCl on the vascular system may be potentiated.
No carcinogenesis or impairment of fertility studies have been carried out with levalbuterol HCl alone. However, racemic albuterol sulfate has been evaluated for its carcinogenic potential and ability to impair fertility.
In a 2-year study in Sprague-Dawley rats, racemic albuterol sulfate caused a significant dose-related increase in the incidence of benign leiomyomas of the mesovarium at and above dietary doses of 2 mg/kg (approximately 2 times the maximum recommended daily inhalation dose of levalbuterol HCl for adults and children on a mg/m2 basis). In another study, this effect was blocked by the coadministration of propranolol, a nonselective beta-adrenergic antagonist. In an 18-month study in CD-1 mice, racemic albuterol sulfate showed no evidence of tumorigenicity at dietary doses up to 500 mg/kg (approximately 260 times the maximum recommended daily inhalation dose of levalbuterol HCl for adults and children on a mg/m2 basis). In a 22-month study in the Golden hamster, racemic albuterol sulfate showed no evidence of tumorigenicity at dietary doses up to 50 mg/kg (approximately 35 times the maximum recommended daily inhalation dose of levalbuterol HCl for adults and children on a mg/m2 basis).
Levalbuterol HCl was not mutagenic in the Ames test or the CHO/HPRT Mammalian Forward Gene Mutation Assay. Although levalbuterol HCl has not been tested for clastogenicity, racemic albuterol sulfate was not clastogenic in a human peripheral lymphocyte assay or in an AH1 strain mouse micronucleus assay. Reproduction studies in rats using racemic albuterol sulfate demonstrated no evidence of impaired fertility at oral doses up to 50 mg/kg (approximately 55 times the maximum recommended daily inhalation dose of levalbuterol HCl for adults on a mg/m2 basis).
A reproduction study in New Zealand White rabbits demonstrated that levalbuterol HCl was not teratogenic when administered orally at doses up to 25 mg/kg (approximately 110 times the maximum recommended daily inhalation dose of levalbuterol HCl for adults on a mg/m2 basis). However, racemic albuterol sulfate has been shown to be teratogenic in mice and rabbits. A study in CD-1 mice given racemic albuterol sulfate subcutaneously showed cleft palate formation in 5 of 111 (4.5%) fetuses at 0.25 mg/kg (less than the maximum recommended daily inhalation dose of levalbuterol HCl for adults on a mg/m2 basis) and in 10 of 108 (9.3%) fetuses at 2.5 mg/kg (approximately equal to the maximum recommended daily inhalation dose of levalbuterol HCl for adults on a mg/m2 basis). The drug did not induce cleft palate formation when administered subcutaneously at a dose of 0.025 mg/kg (less than the maximum recommended daily inhalation dose of levalbuterol HCl for adults on a mg/m2 basis). Cleft palate also occurred in 22 of 72 (30.5%) fetuses from females treated subcutaneously with 2.5 mg/kg of isoproterenol (positive control).
A reproduction study in Stride Dutch rabbits revealed cranioschisis in 7 of 19 (37%) fetuses when racemic albuterol sulfate was administered orally at a dose of 50 mg/kg (approximately 110 times the maximum recommended daily inhalation dose of levalbuterol HCl for adults on a mg/m2 basis).
A study in which pregnant rats were dosed with radiolabeled racemic albuterol sulfate demonstrated that drug-related material is transferred from the maternal circulation to the fetus.
There are no adequate and well-controlled studies of Xopenex Inhalation Solution in pregnant women. Because animal reproduction studies are not always predictive of human response, Xopenex Inhalation Solution should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
During marketing experience of racemic albuterol, various congenital anomalies, including cleft palate and limb defects, have been rarely reported in the offspring of patients being treated with racemic albuterol. Some of the mothers were taking multiple medications during their pregnancies. No consistent pattern of defects can be discerned, and a relationship between racemic albuterol use and congenital anomalies has not been established.
Because of the potential for beta-adrenergic agonists to interfere with uterine contractility, the use of Xopenex Inhalation Solution for the treatment of bronchospasm during labor should be restricted to those patients in whom the benefits clearly outweigh the risk.
Levalbuterol HCl has not been approved for the management of preterm labor. The benefit:risk ratio when levalbuterol HCl is administered for tocolysis has not been established. Serious adverse reactions, including maternal pulmonary edema, have been reported during or following treatment of premature labor with beta2-agonists, including racemic albuterol.
Plasma levels of levalbuterol after inhalation of therapeutic doses are very low in humans, but it is not known whether levalbuterol is excreted in human milk.
Because of the potential for tumorigenicity shown for racemic albuterol in animal studies and the lack of experience with the use of Xopenex Inhalation Solution by nursing mothers, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. Caution should be exercised when Xopenex Inhalation Solution is administered to a nursing woman.
The safety and efficacy of Xopenex (levalbuterol HCl) Inhalation Solution have been established in pediatric patients 6 years of age and older in one adequate and well-controlled clinical trial (see CLINICAL PHARMACOLOGY; Pharmacokinetics and Clinical Trials ). Use of Xopenex in children is also supported by evidence from adequate and well-controlled studies of Xopenex in adults, considering that the pathophysiology and the drug's exposure level and effects in pediatric and adult patients are substantially similar. Safety and effectiveness of Xopenex in pediatric patients below the age of 6 years have not been established.
Data on the use of Xopenex in patients 65 years of age and older are very limited. A very small number of patients 65 years of age and older were treated with Xopenex Inhalation Solution in a 4-week clinical study (see CLINICAL PHARMACOLOGY; Clinical Trials ) (n=2 for 0.63 mg and n=3 for 1.25 mg). In these patients, bronchodilation was observed after the first dose on day 1 and after 4 weeks of treatment. There are insufficient data to determine if the safety and efficacy of Xopenex Inhalation Solution are different in patients < 65 years of age and patients 65 years of age and older. In general, patients 65 years of age and older should be started at a dose of 0.63 mg of Xopenex Inhalation Solution. If clinically warranted due to insufficient bronchodilator response, the dose of Xopenex Inhalation Solution may be increased in elderly patients as tolerated, in conjunction with frequent clinical and laboratory monitoring, to the maximum recommended daily dose (see DOSAGE AND ADMINISTRATION ).
XOPENEX ADVERSE REACTIONS
Adverse events reported in ≥2% of patients receiving Xopenex Inhalation Solution or racemic albuterol and more frequently than in patients receiving placebo in a 4-week, controlled clinical trial are listed in Table 3 .
| Percent of Patients | ||||
| Body System Preferred Term |
Placebo (n=75) |
Xopenex 1.25 mg (n=73) |
Xopenex 0.63 mg (n=72) |
Racemic albuterol 2.5 mg (n=74) |
| Body as a Whole | ||||
| Allergic reaction | 1.3 | 0 | 0 | 2.7 |
| Flu syndrome | 0 | 1.4 | 4.2 | 2.7 |
| Accidental injury | 0 | 2.7 | 0 | 0 |
| Pain | 1.3 | 1.4 | 2.8 | 2.7 |
| Back pain | 0 | 0 | 0 | 2.7 |
| Cardiovascular System | ||||
| Tachycardia | 0 | 2.7 | 2.8 | 2.7 |
| Migraine | 0 | 2.7 | 0 | 0 |
| Digestive System | ||||
| Dyspepsia | 1.3 | 2.7 | 1.4 | 1.4 |
| Musculoskeletal System | ||||
| Leg cramps | 1.3 | 2.7 | 0 | 1.4 |
| Central Nervous System | ||||
| Dizziness | 1.3 | 2.7 | 1.4 | 0 |
| Hypertonia | 0 | 0 | 0 | 2.7 |
| Nervousness | 0 | 9.6 | 2.8 | 8.1 |
| Tremor | 0 | 6.8 | 0 | 2.7 |
| Anxiety | 0 | 2.7 | 0 | 0 |
| Respiratory System | ||||
| Cough increased | 2.7 | 4.1 | 1.4 | 2.7 |
| Infection viral | 9.3 | 12.3 | 6.9 | 12.2 |
| Rhinitis | 2.7 | 2.7 | 11.1 | 6.8 |
| Sinusitis | 2.7 | 1.4 | 4.2 | 2.7 |
| Turbinate edema | 0 | 1.4 | 2.8 | 0 |
The incidence of certain systemic beta-adrenergic adverse effects (e.g., tremor, nervousness) was slightly less in the Xopenex 0.63 mg group compared with the other active treatment groups. The clinical significance of these small differences is unknown.
Changes in heart rate 15 minutes after drug administration and in plasma glucose and potassium 1 hour after drug administration on day 1 and day 29 were clinically comparable in the Xopenex 1.25 mg and racemic albuterol 2.5 mg groups (see Table 4 ). Changes in heart rate and plasma glucose were slightly less in the Xopenex 0.63 mg group compared with the other active treatment groups (see Table 4 ). The clinical significance of these small differences is unknown. After 4 weeks, effects on heart rate, plasma glucose, and plasma potassium were generally diminished compared with day 1 in all active treatment groups.
| Treatment | Mean Changes (day 1) | ||
| Heart Rate (bpm) |
Glucose (mg/dL) |
Potassium (mEq/L) |
|
| Xopenex 0.63 mg, n=72 | 2.4 | 4.6 | –0.2 |
| Xopenex 1.25 mg, n=73 | 6.9 | 10.3 | –0.3 |
| Racemic albuterol 2.5 mg, n=74 | 5.7 | 8.2 | –0.3 |
| Placebo, n=75 | –2.8 | –0.2 | –0.2 |
No other clinically relevant laboratory abnormalities related to administration of Xopenex Inhalation Solution were observed in this study.
In the clinical trials, a slightly greater number of serious adverse events, discontinuations due to adverse events, and clinically significant ECG changes were reported in patients who received Xopenex 1.25 mg compared with the other active treatment groups.
The following adverse events, considered potentially related to Xopenex, occurred in less than 2% of the 292 subjects who received Xopenex and more frequently than in patients who received placebo in any clinical trial:
| Body as a Whole: | chills, pain, chest pain |
| Cardiovascular System: | ECG abnormal, ECG change, hypertension, hypotension, syncope |
| Digestive System: | diarrhea, dry mouth, dry throat, dyspepsia, gastroenteritis, nausea |
| Hemic and Lymphatic System: | lymphadenopathy |
| Musculoskeletal System: | leg cramps, myalgia |
| Nervous System: | anxiety, hypesthesia of the hand, insomnia, paresthesia, tremor |
| Special Senses: | eye itch |
The following events, considered potentially related to Xopenex, occurred in less than 2% of the treated subjects but at a frequency less than in patients who received placebo: asthma exacerbation, cough increased, wheezing, sweating, and vomiting.
XOPENEX ADVERSE REACTIONS
Adverse events reported in ≥2% of patients in any treatment group and more frequently than in patients receiving placebo in a 3-week, controlled clinical trial are listed in Table 5 .
| Percent of Patients | |||||
| Body System Preferred Term |
Placebo (n=59) |
Xopenex 0.31 mg (n=66) |
Xopenex 0.63 mg (n=67) |
Racemic albuterol 1.25 mg (n=64) |
Racemic albuterol 2.5 mg (n=60) |
| Body as a Whole | |||||
| Abdominal pain | 3.4 | 0 | 1.5 | 3.1 | 6.7 |
| Accidental injury | 3.4 | 6.1 | 4.5 | 3.1 | 5.0 |
| Asthenia | 0 | 3.0 | 3.0 | 1.6 | 1.7 |
| Fever | 5.1 | 9.1 | 3.0 | 1.6 | 6.7 |
| Headache | 8.5 | 7.6 | 11.9 | 9.4 | 3.3 |
| Pain | 3.4 | 3.0 | 1.5 | 4.7 | 6.7 |
| Viral Infection | 5.1 | 7.6 | 9.0 | 4.7 | 8.3 |
| Digestive System | |||||
| Diarrhea | 0 | 1.5 | 6.0 | 1.6 | 0 |
| Hemic and Lymphatic | |||||
| Lymphadenopathy | 0 | 3.0 | 0 | 1.6 | 0 |
| Musculoskeletal System | |||||
| Myalgia | 0 | 0 | 1.5 | 1.6 | 3.3 |
| Respiratory System | |||||
| Asthma | 5.1 | 9.1 | 9.0 | 6.3 | 10.0 |
| Pharyngitis | 6.8 | 3.0 | 10.4 | 0 | 6.7 |
| Rhinitis | 1.7 | 6.1 | 10.4 | 3.1 | 5.0 |
| Skin and Appendages | |||||
| Eczema | 0 | 0 | 0 | 0 | 3.3 |
| Rash | 0 | 0 | 7.5 | 1.6 | 0 |
| Urticaria | 0 | 0 | 3.0 | 0 | 0 |
| Special Senses | |||||
| Otitis Media | 1.7 | 0 | 0 | 0 | 3.3 |
|
Note: Subjects may have more than one adverse event per body system and preferred term. |
Changes in heart rate, plasma glucose, and serum potassium are shown in Table 6 . The clinical significance of these small differences is unknown.
| Treatment | Mean Changes (Day 1) | ||
| Heart Rate (bpm) |
Glucose (mg/dL) |
Potassium (mEq/L) |
|
| Xopenex 0.31 mg, n=66 | 0.8 | 4.9 | –0.31 |
| Xopenex 0.63 mg, n=67 | 6.7 | 5.2 | –0.36 |
| Racemic albuterol 1.25 mg, n=64 | 6.4 | 8.0 | –0.27 |
| Racemic albuterol 2.5 mg, n=60 | 10.9 | 10.8 | –0.56 |
| Placebo, n=59 | –1.8 | 0.6 | –0.05 |
| Mean Changes (Day 21) | |||
| Treatment | Heart Rate (bpm) |
Glucose (mg/dL) |
Potassium (mEq/L) |
| Xopenex 0.31 mg, n= 60 | 0 | 2.6 | –0.32 |
| Xopenex 0.63 mg, n=66 | 3.8 | 5.8 | –0.34 |
| Racemic albuterol 1.25 mg, n= 62 | 5.8 | 1.7 | –0.18 |
| Racemic albuterol 2.5 mg, n= 54 | 5.7 | 11.8 | –0.26 |
| Placebo, n= 55 | –1.7 | 1.1 | –0.04 |
SPL UNCLASSIFIED
In addition to the adverse events reported in clinical trials, the following adverse events have been observed in postapproval use of Xopenex Inhalation Solution. These events have been chosen for inclusion due to their seriousness, their frequency of reporting, or their likely beta-mediated mechanism: angioedema, anaphylaxis, arrhythmias (including atrial fibrillation, supraventricular tachycardia, extrasystoles), asthma, chest pain, cough increased, dyspnea, metabolic acidosis, nausea, nervousness, rash, tachycardia, tremor, urticaria. Because these events have been reported spontaneously from a population of unknown size, estimates of frequency cannot be made.
OVERDOSAGE
The expected symptoms with overdosage are those of excessive beta-adrenergic receptor stimulation and/or occurrence or exaggeration of any of the symptoms listed under ADVERSE REACTIONS , e.g., seizures, angina, hypertension or hypotension, tachycardia with rates up to 200 beats/min., arrhythmias, nervousness, headache, tremor, dry mouth, palpitation, nausea, dizziness, fatigue, malaise, and sleeplessness. Hypokalemia also may occur. As with all sympathomimetic medications, cardiac arrest and even death may be associated with the abuse of Xopenex Inhalation Solution. Treatment consists of discontinuation of Xopenex Inhalation Solution together with appropriate symptomatic therapy. The judicious use of a cardioselective beta-receptor blocker may be considered, bearing in mind that such medication can produce bronchospasm. There is insufficient evidence to determine if dialysis is beneficial for overdosage of Xopenex Inhalation Solution.
The intravenous median lethal dose of levalbuterol HCl in mice is approximately 66 mg/kg (approximately 70 times the maximum recommended daily inhalation dose of levalbuterol HCl for adults and children on a mg/m2 basis). The inhalation median lethal dose has not been determined in animals.
DOSAGE & ADMINISTRATION
Children 6–11 years old: The recommended dosage of Xopenex (levalbuterol HCl) Inhalation Solution for patients 6–11 years old is 0.31 mg administered three times a day, by nebulization. Routine dosing should not exceed 0.63 mg three times a day.
Adults and Adolescents ≥12 years old: The recommended starting dosage of Xopenex (levalbuterol HCl) Inhalation Solution for patients 12 years of age and older is 0.63 mg administered three times a day, every 6 to 8 hours, by nebulization.
Patients 12 years of age and older with more severe asthma or patients who do not respond adequately to a dose of 0.63 mg of Xopenex Inhalation Solution may benefit from a dosage of 1.25 mg three times a day.
Patients receiving the highest dose of Xopenex Inhalation Solution should be monitored closely for adverse systemic effects, and the risks of such effects should be balanced against the potential for improved efficacy.
The use of Xopenex Inhalation Solution can be continued as medically indicated to control recurring bouts of bronchospasm. During this time, most patients gain optimal benefit from regular use of the inhalation solution.
If a previously effective dosage regimen fails to provide the expected relief, medical advice should be sought immediately, since this is often a sign of seriously worsening asthma that would require reassessment of therapy.
The drug compatibility (physical and chemical), efficacy, and safety of Xopenex Inhalation Solution when mixed with other drugs in a nebulizer have not been established.
The safety and efficacy of Xopenex Inhalation Solution have been established in clinical trials when administered using the PARI LC Jet™ and PARI LC Plus™ nebulizers, and the PARI Master® Dura-Neb® 2000 and Dura-Neb® 3000 compressors. The safety and efficacy of Xopenex Inhalation Solution when administered using other nebulizer systems have not been established.
HOW SUPPLIED
Xopenex (levalbuterol HCl) Inhalation Solution is supplied in 3 mL unit-dose, low-density polyethylene (LDPE) vials as a clear, colorless, sterile, preservative-free, aqueous solution, in three different strengths of levalbuterol (0.31 mg, 0.63 mg, 1.25 mg). Each strength of Xopenex Inhalation Solution is available in a shelf-carton containing one or more foil pouches, each containing 12 unit-dose LDPE vials.
Xopenex (levalbuterol HCl) Inhalation Solution, 0.31 mg (foil pouch label color green) contains 0.31 mg of levalbuterol (as 0.36 mg of levalbuterol HCl) and is available in cartons of 24 unit-dose LDPE vials (NDC 63402-511-24).
Xopenex (levalbuterol HCl) Inhalation Solution, 0.63 mg (foil pouch label color yellow) contains 0.63 mg of levalbuterol (as 0.73 mg of levalbuterol HCl) and is available in cartons of 24 unit-dose LDPE vials (NDC 63402-512-24).
Xopenex (levalbuterol HCl) Inhalation Solution, 1.25 mg (foil pouch label color red) contains 1.25 mg of levalbuterol (as 1.44 mg of levalbuterol HCl) and is available in cartons of 24 unit-dose LDPE vials (NDC 63402-513-24).
Xopenex (levalbuterol HCl) Inhalation Solution is also available as a concentrate in individually pouched 0.5 mL unit-dose vials containing 1.25 mg of levalbuterol (NDC 63402-515-30).
Store Xopenex (levalbuterol HCl) Inhalation Solution in the protective foil pouch at 20-25°C (68-77°F) [see USP Controlled Room Temperature]. Protect from light and excessive heat. Keep unopened vials in the foil pouch. Once the foil pouch is opened, the vials should be used within 2 weeks. Vials removed from the pouch, if not used immediately, should be protected from light and used within 1 week. Discard any vial if the solution is not colorless.
SUNOVION
Manufactured for:
Sunovion Pharmaceuticals Inc.
Marlborough, MA 01752 USA
For customer service, call 1-888-394-7377.
To report adverse events, call 1-877-737-7226.
For medical information, call 1-800-739-0565.
Sunovion Pharmaceuticals Inc. was formerly Sepracor Inc.
September 2012
400437R08
PHARMACIST — DETACH HERE AND GIVE INSTRUCTIONS TO PATIENT
---------------------------------------------------------------------------------------------------------------
SPL PATIENT PACKAGE INSERT
Xopenex ®
(levalbuterol HCl)
Inhalation Solution
0.31 mg*, 0.63 mg*, 1.25 mg*
3 mL Unit-Dose Vials
*Potency expressed as levalbuterol
Read complete instructions carefully before using.

Figure 1 |
|

Figure 2 
Figure 3 
Figure 4 |
|
Note: Xopenex (levalbuterol HCl) Inhalation Solution should be used in a nebulizer only under the direction of a physician. More frequent administration or higher doses are not recommended without first discussing with your doctor. This solution should not be injected or administered orally. Protect from light and excessive heat. Store in the protective foil pouch at 20-25°C (68-77°F) [see USP Controlled Room Temperature]. Keep unopened vials in the foil pouch. Once the foil pouch is opened, the vials should be used within 2 weeks. Vials removed from the pouch, if not used immediately, should be protected from light and used within 1 week. Discard any vial if the solution is not colorless.
The safety and effectiveness of Xopenex Inhalation Solution have not been determined when one or more drugs are mixed with it in a nebulizer. Check with your doctor before mixing any medications in your nebulizer.
SUNOVION
Manufactured for:
Sunovion Pharmaceuticals Inc.
Marlborough, MA 01752 USA
For customer service, call 1-888-394-7377.
To report adverse events, call 1-877-737-7226.
For medical information, call 1-800-739-0565.
Sunovion Pharmaceuticals Inc. was formerly Sepracor Inc.
September 2012
400437R08
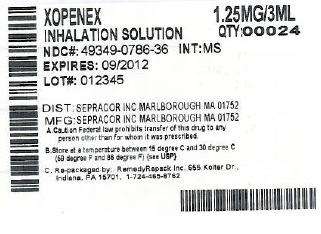
PACKAGE LABEL.PRINCIPAL DISPLAY PANEL SECTION
DRUG: Xopenex
GENERIC: levalbuterol hydrochloride
DOSAGE: SOLUTION
ADMINSTRATION: RESPIRATORY (INHALATION)
NDC: 49349-768-36
ACTIVE INGREDIENT(S):
- levalbuterol hydrochloride 1.25mg in 3mL
INACTIVE INGREDIENT(S):
- nitrogen
- water
- sodium chloride
- sulfuric acid
PACKAGING: 3 mL in 1 VIAL, SINGLE-DOSE

/>
Xopenexlevalbuterol hydrochloride SOLUTION
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||